Airway Management Guidelines: Why Are They Important?
Share this step
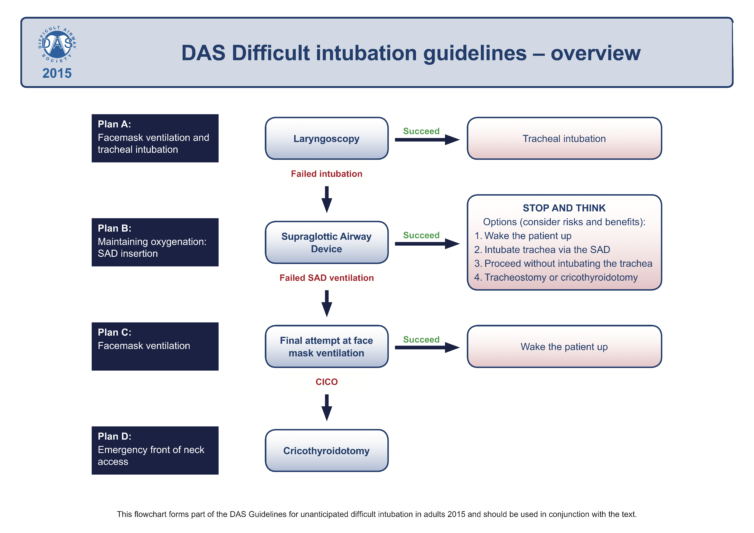
In this article Prof Chris Frerk, Consultant Anaesthetist at Northampton General Hospital and author of the Difficult Airway Society 2015 guidelines for the management of the unanticipated difficult airway in adults, explains how guidelines, algorithms and cognitive aids are helpful in challenging situations.
Looking after airways is usually easy once you have had some training. Anaesthetists place supraglottic airway devices every day without difficulty. We place tubes in tracheas safely and correctly every day. It is easy to do these things 99 times out of 100.
But 1 time in 100 it is difficult to place a supraglottic airway. And 1 time in 100 it is difficult to place a tube in the trachea. This happens because of the patient’s anatomy. It happens to very experienced clinicians as well as to newly trained healthcare workers. It happens about once a year. It happens when you least expect it.
Imagine what it might feel like when something that you usually do well goes wrong one day. Imagine what it might feel like when the patient’s life is at risk because you cannot get oxygen to their lungs.
This is where guidelines are helpful. Someone else has already done the thinking for you. There is a plan of what to do if things go wrong. It is the same plan every day in every hospital. Most days you don’t need to use the plan because most days everything goes well.
- If you work with an assistant they will know the guidelines too. You can work well together better because you have both learned the same plan.
- When another person arrives to help they will also know the guidelines. You can work well together because you have all learned the same plan.
- All the equipment you want will be there because the hospital has prepared for the plan.
- Bag and mask ventilation
- Ventilation through a supraglottic airway
- Ventilation through a tracheal tube
Look at Plan A in the DAS guideline diagram:
If you cannot intubate the trachea do not worry.
If you cannot intubate the trachea follow the guidelines.
Even if bag and mask ventilation is easy it is time to move on to plan B.
Look at Plan B in the DAS guideline diagram:
It is extremely rare for both Plan A and Plan B to fail. It probably happens less than one time in 20,000. But if it happens to you with a patient next week there is no need to worry as long as you follow the guidelines. It is as easy as “ABC”. If Plan A and Plan B have not worked then we use Plan C.
Look at Plan C in the DAS guidelines diagram:
There is one other plan in the guidelines. That is Plan D:
Because Plan A, B and C work so well you will probably never need to use Plan D. Most anaesthetists will never need to use Plan D.
If you are able to use Plan A, B and C you will be able to look after patients airways safely. And you need to practice Plan D, just in case you need to use it one day in the future. If bag and mask ventilation fails, tracheal intubation fails, supraglottic airway fails and the patient is becoming hypoxic then you have to go to Plan D.
References
Share this

Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free












