How Does Vaccination Work?
Vaccinations are part of the success story of modern medicine, and their discovery has saved numerous lives. However, the long and insistent work of many researchers was needed to get that far.
History of vaccinations
The father of vaccination – at least from a Western point of view – is Edward Jenner (1749-1823), an English country physician. At his time, smallpox (Variola vera) was a deadly disease which killed approximately 30% of the patients affected. Already Chinese physicians tried to ‘inoculate’ or ‘variolate’ patients with secretions of lesions: crusts of smallpox lesions were crushed and blown into the nose, or lesional secretions were scratched into the skin. This method was introduced in Europe in the 18th century by Lady Mary Montagu. Most individuals survived this treatment, yet a few percent died either from the transmitted smallpox or from other infections caused by non-sterile instruments. At that time, it was already known that dairymaids who had been first infected with the cowpox virus, were later protected from smallpox, caused by a related virus. In 1796, the English physician Edward Jenner inoculated the 8 year-old James Phipps with material from cowpox lesions of a dairymaid, freshly affected with this disease harmless for humans. Two months later, he inoculated the 8 year-old with smallpox material and, luckily, the boy did not develop any symptoms.
The world’s first vaccine
In 1721, Lady Mary Wortley Montagu had imported variolation to Britain after having observed it in Constantinople. Variolation, which used smallpox to create an immunity to itself, was already a standard practice but involved serious risks.
In the years following, several investigators successfully tested in humans a cowpox vaccine against smallpox, but it was not until Jenner’s work that the procedure became widely understood.

14 May 1796, Edward Jenner performed his first vaccination on James Phipps, a boy of age 8.
After some more successful cases, Jenner published his observations and termed the procedure ‘vaccination’, derived from the Latin word ‘vacca’ for ‘cow’. Even if there were many initial concerns and criticism, the principle of vaccination rapidly spread throughout Europe. This was the first successful procedure to prevent a frequently mortal disease. Still, it took more than one hundred years to establish widespread smallpox vaccination programs in Western countries. Finally, the efforts of the WHO resulted in the eradication of smallpox in 1977, nearly two centuries after the discovery by Edward Jenner.
Principles of vaccinations
The immunology of today describes the processes involved in vaccination more precisely than this was possible at the beginning of the 20th century. There are important differences between bacterial and viral infections. Bacteria are single cells that can replicate and grow in a suitable environment, even on necrotic, ie dead tissues. Viruses contain just their genetic code in an envelope and need to enter a living host cell to replicate. Most vaccines work best against proteins, ie toxins produced by bacteria for example tetanus or diphtheria or proteins from viral envelopes, eg in hepatitis. If we want to understand why vaccination was effective, we first need to recognize that an organism is able to create defence cells, that ‘remember’ the specifics of an intruder. Second, we need to recap how these memory cells are functional in vaccination. Some viruses may evade the immune defense because they mutate or the produced antibodies are not very effective.
The organism produces specific cells that help address invading germs. Before the intrusion, these cells – B cells and T cells – exist in a so-called naïve state. As soon as a pathogen – the infectious agent – is detected, cells start transformation in order to become operative particularly against this kind of pathogen. B cells become plasma cells that emit antibodies specifically tuned to the intruder’s antigen. Thus, the cells disarm a pathogen quite effectively as the antibodies dock to the pathogen’s antigen. At the same time the so-called B memory cells are produced. These are cells that remember the specifics of the pathogen and can react much more quickly if an attack by the same pathogen occurs.
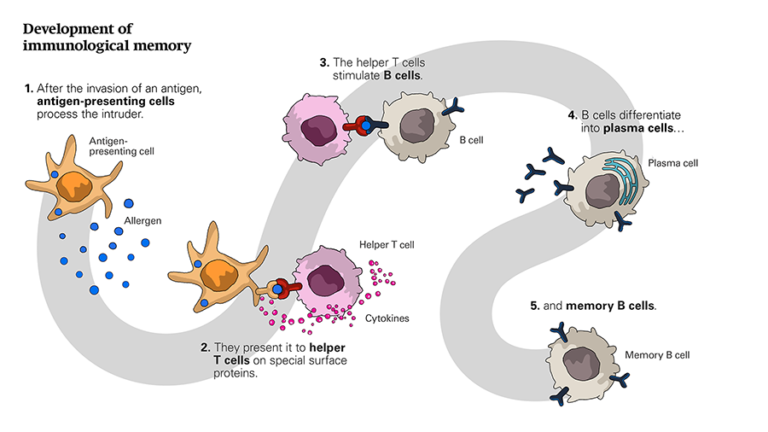 Development of immunological memory. (click to enlarge)
Development of immunological memory. (click to enlarge)
Basically, vaccination helps to build an immune defence against bacterial microbes and particularly their toxins, or against viral envelope structures. Toxins are venomous substances produced within living cells and organisms. One form of vaccination introduces an inactivated toxin – a so-called toxoid – into the organism. After the necessary time the vaccinated organism mounts the first antibody response. Through this, memory cells are formed. If the natural toxin later affects the body, the specific immune response is not only quicker but it has also gained in scope. The vaccination thus enlarges the acquired immunity of an organism.
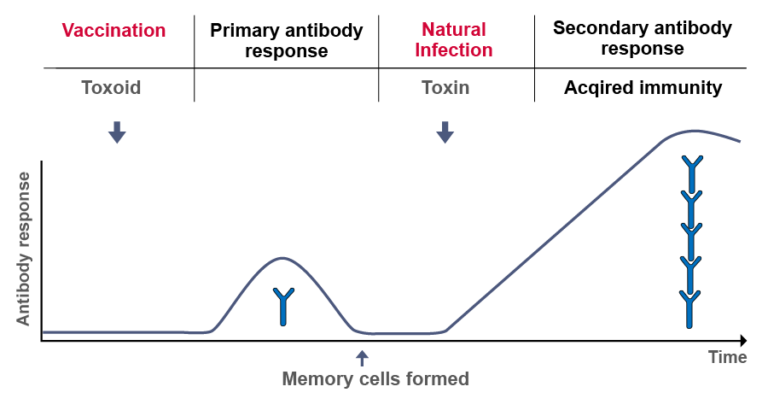 Active immunisation.
Active immunisation.
This is the basic process of active vaccination. However, today, we know that immunisation can happen actively or passively through an either natural or artificially-induced mechanism.
- Natural active immunity: In some diseases, a single natural infection results in a lifelong immunity (eg chickenpox), although a secondary local outbreak called ‘shingles’ is possible. This is naturally acquired active immunity. More specifically, the immune system activates memory B and T cells to produce antibodies and T effector cells preventing a second outbreak of the disease.
- Artificial active immunity: Active vaccination involves the induction of pathogen-specific antibodies and/or effector cells. This can be achieved by live, attenuated, or inactivated pathogens or purified antigens. This type of vaccination is for example used to protect patients against tetanus toxin through induction of protective anti-tetanus antibodies by an attenuated tetanus toxoid.
- Natural passive immunity: An example for natural passive immunity is the transfer of antibodies from mother-to-child, through the placenta and later through breastfeeding. Passive immunisation lasts for several weeks to some months only.
- Artificial passive immunity: Artificially-acquired passive immunity is the transfer of antibodies from another human or another species to an individual. This results in immediate but short-lived immunity, because the antibodies are not produced by the individuals themselves. It is for example used in an unvaccinated person, if bitten by a rabid dog. Anti-rabies antibodies and rabies vaccine are given in parallel, otherwise the patient would likely die before he has produced sufficient protective antibodies.
With this in mind you might want to explore the history of vaccines. Think about the assumptions, concepts, or questions that drove these discoveries forward.
Share this
Allergies: When the Immune System Backfires

Allergies: When the Immune System Backfires


Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free







