I Have a Runny Nose—Is It COVID-19?

Share this step
In this article, we’ll discuss the key clinical features of COVID-19. By the end of this step, you should have updated your knowledge on the key signs of COVID-19 and begun to reflect how the clinical appearance of the disease could influence disease surveillance and diagnosis.
Clinical Features of COVID 19
COVID-19 was first widely reported in late December 2019, when a series of cases of ‘atypical pneumonia’ was reported in Wuhan, China1. ‘Atypical pneumonia’ means a pneumonia, or lung infection, not caused by the usual infectious agents, such as influenza. Early on, the features of COVID-19 cases that sparked attention were how quickly patients developed the severe respiratory disease. That is how quickly they progressed from mild signs including fever, a dry cough, and shortness of breath, to acute respiratory distress, which is a recognised clinical syndrome involving severely compromised respiratory function2-4. Importantly, a large majority of the early cases had strong links to the Huanan Seafood Market in Wuhan, suggesting a common source of these unusual infections3. Together, these unusual clinical signs, severe and rapid disease progression, common epidemiological connection to the Huanan Market, and negative tests to other common causes of respiratory disease, alerted people to the threat of a new infectious disease.
These cases appeared in winter in Wuhan when seasonal influenza—which shares some similar signs to COVID-19—is also most common, and some cases were similar to Severe Acute Respiratory Syndrome (SARS), which had appeared in Asia in 2002. However, tests for the coronavirus that causes the ‘original’ SARS, influenza and other infectious causes of pneumonia were negative. One wonders whether COVID-19 would have been identified so quickly if it had occurred in a country that did not have to respond to SARS in 2002. Would a new, severe disease be more likely to be suspected in a country that responded to a similar outbreak a couple of decades earlier? OR In a country with no direct experience of such an outbreak, making this unusual disease even more noticeable?
Like many diseases, COVID-19 does not produce the same signs in all patients. The following figure shows the frequency of different signs observed in several series of COVID-19 cases reported from China early in the pandemic. Note that fever and cough were very common. How would these signs be distinguished from the numerous causes of these signs in different settings? Remember, it was the rapid progression of many of these cases to severe disease that required hospitalisation, along with the common connection to Huanan Market, that made people suspect an emerging disease. The figure also shows that many patients showed severe changes to the appearance of their lungs on CT scans in two series of cases.
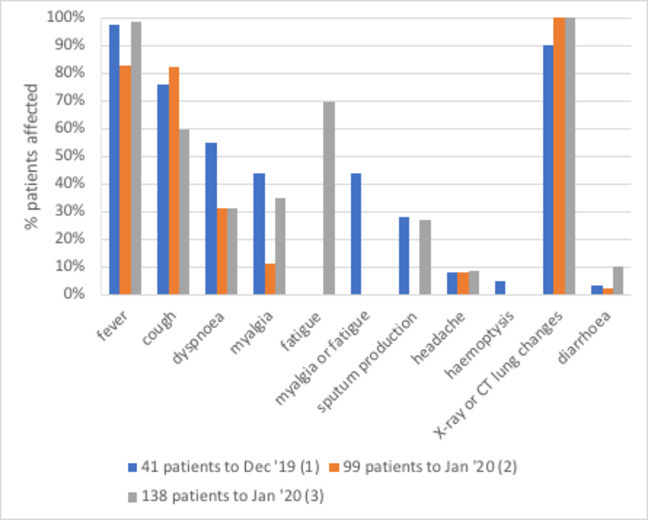
The proportion of people with COVID-19 showing different clinical signs, reported early in the outbreak in China. (Sources: A. Huang et al. (2020)3; B. Chen et al. (2020)2; C. Wang et al. (2020)4)
Although we discussed in the previous step that COVID-19 is caused by a new coronavirus closely related to the one that causes SARS, other coronaviruses are also known to cause much milder respiratory disease, including contributing to the common cold. However, those coronaviruses are more likely to cause a runny nose, sore throat, and/or sneezing, none of which were prominent signs with this new disease. Clinicians might have been alerted to an outbreak of a more serious disease because these first cases had more in common with the emerging diseases SARS or Middle East Respiratory Syndrome (MERS) from recent decades: fever, dry cough, and severe changes seen in X-rays and scans of the lungs. However, about 25% of SARS cases developed diarrhoea, something that we see is uncommon in COVID-19.
The mortality amongst people who contract COVID-19 ranges from <1% to >15%, depending on the setting and characteristics of patients, which is very roughly similar to SARS (6–17%) but less than MERS (20–30+%)5. COVID-19’s case fatality rate, and the rapidity at which some patients deteriorate, was another sign that the world was facing a new and serious infectious disease. The following figure, from the Our World in Data website, shows how the reported case fatality rates vary between countries. You can interact with the graph to display data from other countries or run timelines showing how reported case fatality has varied throughout the pandemic by clicking the link in the caption.
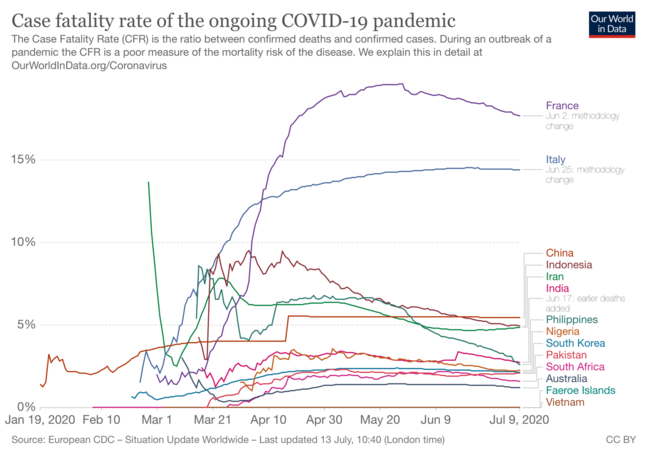 COVID-19 cumulative case fatality rate (the proportion of confirmed cases that die) from January 2020 for selected countries. (Source: OurWorldInData.org)
COVID-19 cumulative case fatality rate (the proportion of confirmed cases that die) from January 2020 for selected countries. (Source: OurWorldInData.org)
After becoming infected, people take 1–14 days to start showing clinical signs; half are showing signs 5-6 days after infection. People may be infectious up to two days before they start showing signs, although most spread is probably from people who are showing signs, even mild ones. Overall, about 20% of patients infected with SARS-CoV-2 require hospitalisation6. Remember from the previous step that SARS-CoV-2 is the specific virus that causes COVID-19.
The clinical signs of the disease and the time it takes for them to develop are key factors health authorities are using to monitor and manage COVID-19. For example, in Victoria, Australia anyone showing signs of recent respiratory disease, including fever, runny nose, dry cough, sore throat or shortness of breath, must avoid contact with other people (including not going to work or school) and seek medical care. People with fever, chills or sweats, cough, sore throat, shortness of breath, runny nose, and loss of sense of smell or taste, regardless of how mild, should get tested and remain in isolation until their result comes back. Of course, there are other reasons for testing including contact with a known or suspect case, your geographical location or travel history; these criteria vary between jurisdictions.
Lastly, about 20% of people with COVID-19 show no clinical signs at all, although they may still infect other people. Maybe this, plus the time before people show signs and the speed of international air travel, is a reason why the disease spread so successfully around the world.
Share this

Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free








