Boosting Health System Surge Capacity
Surge capacity can be defined as the ability to evaluate and care for a markedly increased volume of patients – one that challenges or exceeds normal operating capacity1.
Countries have hugely variable capacity and resources to boost both epidemic preparedness measures prior to an epidemic and surge capacity on the onset of an epidemic. This is owing to a range of factors, including:
- Varying capacity to afford large-scale testing or diagnostics;
- Differing surveillance capacity, along with systems to fast and effectively aggregate reliable country data;
- The extent to which basic infection, prevention, and control (IPC) measures are institutionalised and the availability of IPC supplies;
- The locations of large scale refugee camps, where local health services tend to already be weak;
- Availability of additional resources to fund i.e. intensive care units;
- The absorptive (or spending) capacity of funds across the health system;
- Existing variations inequity of service provision and access to care, particularly for vulnerable groups2.
Expanding Health Worker Capacity
The COVID-19 pandemic has placed immense pressure on the health workforce worldwide, which has been exacerbated by workforce depletion given health professionals themselves are at high risk of being infected. Across Europe – as this image below shows – multiple strategies have been implemented to expand the capacity of the existing workforce, often underpinned by emergency legislation3. Most countries have called upon medical and nursing students to work in clinical practice. Campaigns were launched to bring retired or inactive health professionals back to the workforce – and online portals have been critical to enabling current or inactive health care workers to register their interest in joining the response, to facilitate temporary registration where required, and to match workforce shortages with supply. For many countries though, similar strategies may not be feasible as there may simply not be the available skills or workforce to draw on from within national borders.
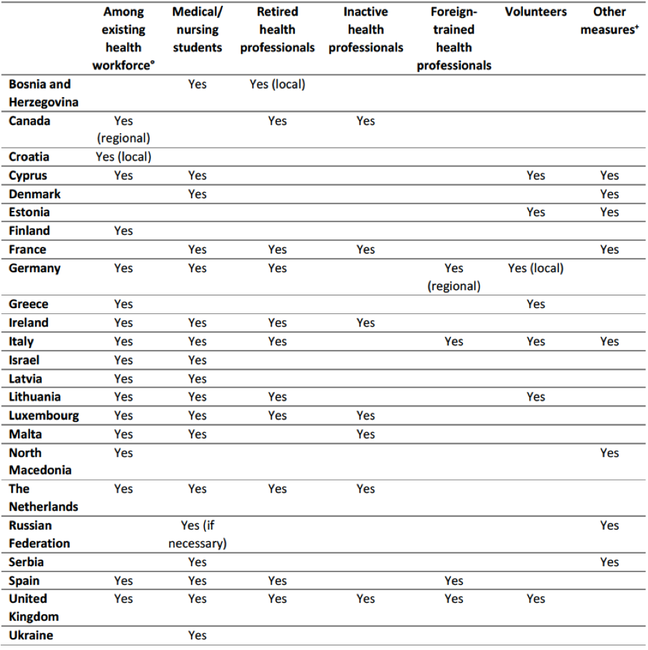 Key strategies implemented across Europe to expand the capacity of the existing health workforce. Source: WHO COVID-19 HRSM, April 2020
Key strategies implemented across Europe to expand the capacity of the existing health workforce. Source: WHO COVID-19 HRSM, April 2020
How are Additional Public Funds Mobilised?
Mounting a strong and fast health system response to an epidemic usually requires additional public funds that can be deployed quickly and transparently4. Without additional resources, the health system will not only struggle to control the epidemic but may also fail to maintain essential health services for other conditions. Simply put, reallocating the existing health budget is not a viable way of addressing the epidemic for two reasons. First, it will not be enough to meet greater demand for health services, including new infrastructure, staff and supplies, outreach to ensure access to testing and treatment for all those who need it, and overtime and supplementary payments for health workers. Second, many countries will have postponed and canceled the delivery of essential health services for other conditions to release capacity to respond to the outbreak in the short run. This is likely to result in unmet needs and adverse effects on health and will require immediate attention once the most urgent phase of the pandemic has passed. Other possible options could include:
- Reprioritising the government budget. Where feasible, additional public funds can be drawn from regular budget sources or national emergency reserves (contingency funds) – though in many countries, these reserves simply won’t be available;
- Removing administrative constraints so that new funds can be deployed quickly. If the governance processes exist, some countries may need to activate exceptional spending procedures in the first phase of the crisis and then formalise these procedures using supplementary budget laws. Declaring a state of emergency can facilitate the release of new funds and speed up public procurement by enabling simplified procedures for trusted suppliers;
- Tracking and reporting spending for transparency and accountability. The fast release of funds and simplified procedures for spending and procurement should be accompanied by mechanisms to prevent fraud and build public trust. Italy, for example, records all expenses in a special COVID-19 account and requires any spending to be published in a manner that’s accessible to the public5.
Removing Financial Barriers to Accessing Health Services
Comparing health spending for COVID-19 across countries at this stage is complicated given the availability of data. Comparisons are also hard to draw given the range of public health strategies deployed and the myriad of contextual factors. While there does seem to be a big variation, there is clearly no right amount of health spending to combat COVID-19.
However, it is important to consider options that may be feasible in some contexts for removing financial barriers for accessing health services6. Households increasingly face financial strain as the COVID-19 outbreak becomes an economic crisis in many countries. If people face concerns about health care affordability, they may delay seeking treatment or be prevented from obtaining the services they need, making the outbreak harder to control. Options could include:
- Suspending all user charges, including co-payments for non-COVID-19 health services;
- Extending entitlement to publicly financed health services to everyone, regardless of residence or insurance status i.e. migrants, refugees, asylum seekers and other non-residents;
- Providing people with income support (multi-purpose cash transfers) i.e. for food and other basic needs or to help alleviate the indirect costs of seeking health care, such as transport costs and lost labour time.
Finally, it is important to emphasise that health and economic shocks do not affect people equally. Some people are systematically more likely than others to experience financial barriers to access, including migrants, people living in poverty, those who have lost work and people in informal or non-stable work. Inequities and inequalities will become further pronounced through the continuing and ever-developing era of COVID-19 and so it is important to identify the people and groups who are most in need. This is a topic area we will explore in more depth in Week 3.
Let’s now take these broad level reflections when examining a country-specific response to COVID-19, in the next step.
Share this

Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free








