Preventing Diabetic Eye Disease: The Public Health Approach

Share this step
This article outlines the public health strategies used to prevent diabetic eye disease. These strategies must be directed at all the healthcare pathways used by people with diabetes and carried out in partnership with the wider diabetes management programme. As you read, consider how each of these strategies are provided in your setting. Who is best placed to implement primary prevention in your setting? Share your view in the Comments.
This article is adapted from: Ockrim Z. Why does diabetic retinopathy happen, and how can we stop it? Community Eye Heal J. 2011;24(75):4.
Table. Public health control of visual impairment from diabetes
| Public health strategy | Who directed towards | Activities & interventions |
|---|---|---|
| Primary prevention: Interventions BEFORE any diabetes occurs | The whole population | Health promotion to raise awareness and lifestyle changes – good nutrition, exercise, quit smoking, avoidance of obesity. |
| Secondary prevention: Interventions to identify POTENTIAL to develop diabetic eye disease (pre-symptomatic) and provide prompt treatment | People with diabetes (the population at risk) | Health education on good diet and managing blood sugar control. Regular monitoring of blood sugars, blood lipids and blood pressure. Early detection through screening programmes for diabetic retinopathy. Laser or antiVEGF treatment to prevent vision loss from sight threatening diabetic retinopathy. |
| Tertiary prevention: Interventions to manage SYMPTOMATIC diabetic eye disease (visual impairment) | People with complications of diabetes | Treatment to try and restore sight where possible e.g. vitrectomy or cataract surgery. Low vision services and rehabilitation for people whose sight loss cannot be treated. |
Primary prevention: To prevent diabetes
Little can be done to prevent type 1 diabetes. The causes are uncertain and we have no evidence that any intervention can prevent it. Where possible it is important for all health professionals to look out for high risk candidates who have a genetic predisposition to diabetes, the human leukocyte antigens HLA risk, and carry out further investigations when appropriate.
Type 2 diabetes, is often preventable. There is good evidence that lifestyle changes, such as losing weight, increasing physical activity, and eating more fruit and vegetables can lead to a significant reduction in the risk of developing type 2 diabetes.
Because diabetes causes vision loss, eye health workers should work together with existing public health programmes for diabetes and include advice on the importance of diabetes management at the eye clinic. This means taking every opportunity to reinforce health messages about avoiding obesity and taking regular exercise and, where appropriate, advising patients about weight loss and diet. This additional input from specialists might also be valuable to a public health campaign as avoiding blindness can be a powerful motivator for behaviour change.
Effective primary prevention interventions must be:
- Easy to deliver and understand, for example through posters, health talks, TV, radio or text messages.
- Attractive to engage the audience through the use of visual and locally relevant content.
- Social to achieve wide acceptance amongst families and large groups at locally relevant community activities, for example at a church or mosque.
- Timely to coincide with other public health events, service delivery or health camps.
Secondary prevention: To reduce vision loss from diabetic eye disease
Once someone has developed diabetes, it is important to raise their awareness that managing their diabetes will reduce their risk of developing eye complications. The best and most affordable eye care we can provide for people with diabetes is to support them to reduce their risk of diabetic retinopathy (DR) through good control of their blood sugar, blood pressure and blood lipids.
Optimal control of diabetes is achieved through good control of:
- Blood sugars: Glycated haemoglobin (HbA1c) level of between 6.5 and 7%. Note that intensively lowering blood glucose to 6.0% is associated with increased mortality.
- Blood pressure of 140/80 mm Hg or lower
- Blood lipids: Total cholesterol less than 4 mmol/l or low density lipoprotein cholesterol less than 2.0 mmol/l.
Blood sugar control
We have strong evidence that blood sugar control is essential to reduce the risk of diabetic retinopathy.
Type 1 diabetes: The diabetes control and complications trial (DCCT) followed two groups of people with type 1 diabetes. One group was given intensive treatment to control blood sugars, and the other was managed in the usual way. After nine years, the study showed that the intensive treatment group lowered their risk of diabetic retinopathy by 76 percent and the rate of disease progression had reduced by 54 percent amongst those who had some retinopathy at the beginning of the study (Aiello & Edic. 2014).
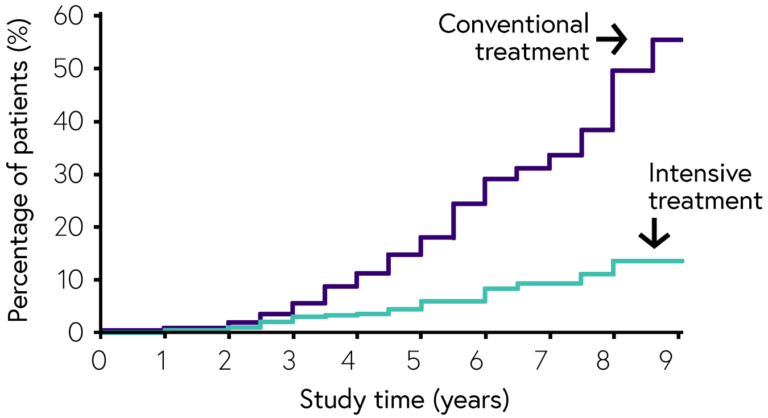
Type 2 diabetes: The United Kingdom Prospective Diabetes Study (UKPDS), published in 1997, showed that good blood sugar control reduced the risk of progression of retinopathy and the need for laser treatment in people with type 2 diabetes. For every 1% decrease in HbA1c there was a reduction of 40% in the development of diabetic retinopathy and a 25% reduction in progression to sight threatening retinopathy and the need for laser treatment (Ting et al. 2016).
Control of blood pressure
In people with diabetes with hypertension (high blood pressure), tight control of blood pressure can reduce the risk of developing diabetic retinopathy. The UKPDS randomly allocated people with diabetes with hypertension into two groups: one with optimal control (which included the addition of medication as required) and the other without tight control or additional drugs. After seven years, there was a 35% reduction in the progression of diabetic retinopathy in the tight blood pressure control group. At nine years, the tight blood pressure control group showed a 47% reduction in the risk of moderate vision loss and a 35% reduction in the need for laser treatment.
The Diabetic Retinopathy Candesartan Trials (DIRECT) were large randomised trials designed to assess whether reducing blood pressure in diabetic patients who did not have hypertension lowered the incidence/ progression of diabetic retinopathy. The trials showed that there was no effect on either the incidence or progression of the disease.
Collaboration with physicians and good communication between eye health workers and patients is essential for successfully implementing secondary prevention. These measures will not only decrease the incidence and progression of diabetic retinopathy. but also the other complications of diabetes, and they will be beneficial for every diabetes patient.
Screening for diabetic retinopathy
Screening is a specific intervention to detect people with disease early and refer them for treatment. Screening is carried out in various ways, by a range of health professionals across different health systems. Appropriate investment and systems are required to implement effective and sustainable screening programmes.
In a population of people with diabetes, the early detection of, and prompt treatment for diabetic retinopathy allows for the prevention of up to 98% of diabetes related vision loss.
The systematic diabetic retinopathy screening programme in Iceland found that the prevalence of blindness within the diabetic population decreased from 2.4% to 0.5% over a 10 year period following the introduction of screening (Ólafsdóttir & Stefánsson. 2007)
Preventing vision loss in a person with diabetes requires good health services that can provide timely treatment and reduce the incidence of vision loss. Other eye conditions linked with diabetes, such as cataract, need to be managed as part of the eye health surgical services and do not require a specific public health intervention.
Tertiary prevention: To manage vision loss due to diabetic eye disease
All tertiary level interventions are directed towards people with diabetes who have vision loss. Action is taken, where possible, to restore or improve their vision as much as possible. When it’s not possible to improve someone’s, action should be taken to provide rehabilitation services and support people to improve their quality of life.
Eye health workers provide routine services for the management of other diabetes related vision impairment – for example managing fluctuating refractive errors. People with diabetes should be made aware of the symptoms and the need to seek services but specific public health approaches are not required here.
Share this
Diabetic Eye Disease: Building Capacity To Prevent Blindness
Diabetic Eye Disease: Building Capacity To Prevent Blindness

Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free







