Ormo case study: Assessing the health system

Share this step
In this step, we see how the toolkit has been used to analyse the current situation for diabetic eye diseases in Ormo across the six interconnected health systems blocks – service delivery, human resources, technology, health information management systems, leadership and governance.
Activities in each block have been considered in three key areas:
- Within the district health centres
- Across the wider diabetic services
- In the eye clinic.
All the key stakeholders in Ormo were involved in discussing and providing information. The brief answers they provided are outlined in the tables below. You can also download this as a PDF.
Service delivery
| Action | Action in Ormo |
|---|---|
| Education about diabetes and the eye | Health centres: Yes Diabetic clinics: Yes Eye clinics: No |
| Education about managing diabetes | Health centres: No Diabetic clinics: Yes Eye clinics: Not actively |
| Screening for diabetes | Health centres: Yes, in all health centres Diabetic clinics: Yes Eye clinics: Yes – only for high risk cases |
| Diagnosis of sight threatening diabetic retinopathy | Health centres: Retinal imaging in two health centres Diabetic clinics: No – symptomatic cases referred to eye clinic Eye clinics: Opportunistic. Long waiting time – over 8 weeks for an appointment. |
| Treatment for sight threatening diabetic retinopathy Options: Laser treatment, antiVEGF injections, vitreoretinal (VR) surgery |
District health centres: Only referral Diabetic clinics: Only referral Eye clinics: Yes – lasers and antiVEGF. VR surgery – referred to national level |
Human resources
| Type of action | Action in Ormo |
|---|---|
| Category of health professional available to care for people with diabetes | District health centres: Primary health workers, nurses Diabetic clinics: Nurses, endocrinologists, physicians Eye clinics: Ophthalmologists, nurses, ophthalmic clinical officers (OCOs) |
| Trained to educate people with diabetes about eye complications | District health centres: No except in two health centres Diabetic clinics: Inadequate Eye clinics: Yes |
| Trained to undertake diabetic retinopathy screening/grading | District health centres: Nurse screener/grader in two health centres Diabetic clinics: None Eye clinics: Opportunistic screening by ophthalmologists |
| Continuing training opportunities for diabetic retinopathy screening | District health centres: Largely not available Diabetic clinics: None Eye clinics: Through external non-governmental organisation (NGO) partner. |
Technology
| Type of action | Action in Ormo |
|---|---|
| Biomedical tests Options: HbA1C, Blood glucose, Blood pressure |
District health centres: Blood glucose, Blood pressure Diabetic clinics: Available – Blood glucose and HbA1C. Blood pressure Eye clinics: Available – Blood glucose and HbA1C |
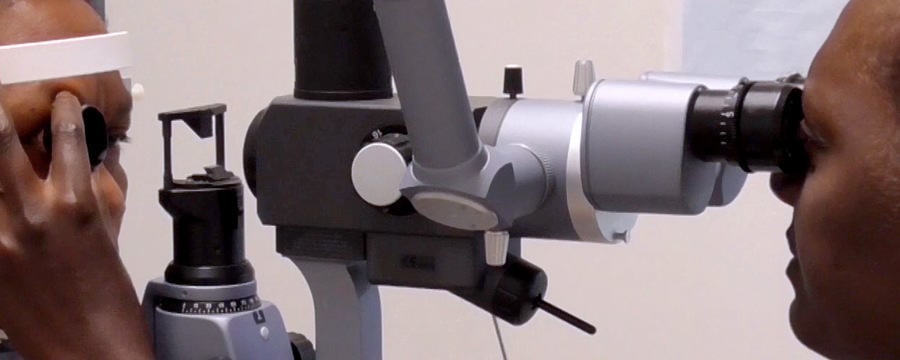
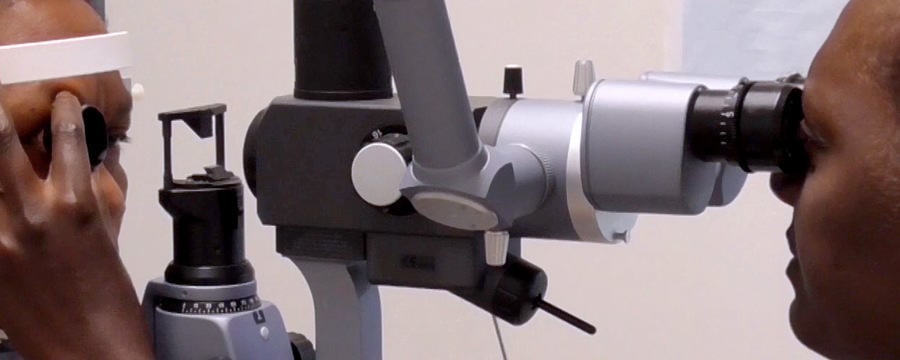
| Ophthalmic/retinal examination Options: Slitlamp, Direct ophthalmoscope, Retinal imaging |
District health centres: Retinal imaging in 2 centres Diabetic clinics: None Eye clinics: Slitlamp, Direct ophthalmoscope, Retinal imaging |
| Treatment Options: Laser treatment, AntiVEGF injections, VR surgery |
In district health centres: None In diabetic clinics: None In eye clinics: 2 lasers, Anti-VEGF (sometimes), VR only in capital city |
Health information management systems
| Type of action | Action in Ormo |
|---|---|
| Database of people with diabetes Options: Name, Paper, Electronic |
District health centres: Paper form in 2 health centres Diabetic clinics: Paper Eye clinics: Paper |
| Information recorded in databases Options: Risk factors, Eye examinations, Level of DR, Follow up |
District health centres: Level of DR in 2 health centres Diabetic clinics: Risk factors, Follow up Eye clinics: Risk factors, Eye examinations, Level of DR, Follow up |
| Available call and recall Options: None, Systematic, Ad hoc mHealth messaging |
District health centres: None Diabetic clinics: None Eye clinics: None |
| Statistics collected and monitored Options: Numbers screened, Number referred to eye clinic, Numbers treated for STDR, Numbers not returning |
District health centres: Numbers screened, Number referred to eye clinic Diabetic clinics: Number referred to eye clinic Eye clinics: Numbers screened, Number referred to eye clinic, Numbers treated for STDR |
| Nationally agreed indicators Options: None, Number of STDR cases referred, Number of patients recalled for screening at regular intervals |
District health centres: None Diabetic clinics: None Eye clinics: None |
| Communications methods with patients Options: Personal record books, Information cards, mHealth: text messaging reminders using mobile phones |
District health centres: Personal record books Diabetic clinics: Personal record books Eye clinics: Personal record books |
Leadership and governance
| Type of action | Action in Ormo |
|---|---|
| Main stakeholders in diabetes and DR services Options: Government, INGO |
District health centres: Government, INGO Diabetic clinics: Government Eye clinics: Government, INGO |
| Leadership for DR services Options: Yes, no, clinical lead |
District health centres: No Diabetic clinics: No Eye clinics: Clinician lead |
| Diabetes Options: As a priority, Has a national plan, Programme with coverage |
District health centres: As a priority Diabetic clinics: As a priority Eye clinics: As a priority |
| Guidelines for DR management Options: None, Formulated but not used , Available and followed occasionally, Available and fully implemented |
District health centres: Available and followed occasionally Diabetic clinics: Available and followed occasionally Eye clinics: Available and followed occasionally |
Finances
| Type of action | Action in Ormo |
|---|---|
| DR screening | District health centres: 100% INGO funded in 2 health centres Diabetic clinics: – Eye clinics: 80% out of pocket for patient. 20% Government subsidy |
| Laser treatment | District health centres: – Diabetic clinics: – Eye clinics: 80% out of pocket for patient. 20% Government subsidy |
| AntiVEGF | District health centres: – Diabetic clinics: – Eye clinics: 80% out of pocket for patient. 20% Government subsidy |
| Eye clinics = Public and private clinics INGO = International non-governmental organisation |
A situation analysis also includes detailed discussions of the health system’s performance and an analysis of the implementation of health sector activities, budgets and finances. This supporting dialogue bring expert views and end user/community opinions together.
Once a situation analysis has been carried out, what else (other than plan the next steps) can be done with this information?
Share this
Diabetic Eye Disease: Building Capacity To Prevent Blindness
Diabetic Eye Disease: Building Capacity To Prevent Blindness

Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free







