Post-operative trichiasis

Share this step
Post-operative trichiasis is when trichiasis is found again in an operated eye of a patient after surgery. It can develop at any time after surgery. Early post-operative trichiasis is probably related to how well the operation was performed, or to wound healing responses. Trichiasis redeveloping may also be related to progressive trachomatous scarring.
Is post-operative trichiasis a problem?
Completely successful trichiasis surgery is defined as:
- No eyelashes rubbing on the eyeball (without the need for epilation or further surgery), and
- No complications (such as infection) and no severe eyelid contour abnormalities, eyelid closure defects, granulomata, or necrosis of lid margin
Post-operative trichiasis is a significant problem for patients and providers because it puts the eye at renewed risk of sight loss.
The proportion of eyes that develop post-operative trichiasis is variable. The incidence (proportion of operated eyes that develop post-operative trichiasis) reported in clinical trials is typically around 20% by one year after surgery. The cumulative incidence rises as the years pass. However, very few operational data have been published from settings in which trachoma elimination programmes are active. It is possible that under programmatic conditions, recurrence rates of trichiasis are even higher and therefore must be monitored.
The four S’s: Key factors associated with post-operative trichiasis
- The severity of a patient’s trichiasis before surgery is a major factor associated with whether trichiasis will redevelop. The more severe the trichiasis before surgery the more likely it is to recur following surgery.
- The surgical method used is important. Some procedures are associated with higher post-operative trichiasis rate than others.
- The skill of the surgeon is very important – research has found that recurrence rates vary significantly between different surgeons. This suggests that there are subtle variations in how the procedure is performed that can influence the outcome.
- Excessive scarring – contraction of the healing tissue from more aggressive post-operative wound healing may be related to some recurrent trichiasis. Post-operative trichiasis developing later may be due to progressive scarring of the conjunctiva from trachoma.
Impact of post-operative trichiasis
Failure to provide a good quality service with acceptable outcomes for patients will undermine progress towards eliminating trachoma. If people with trichiasis see others receiving poor quality surgery, they will be much less inclined to accept the treatment themselves. Good follow up of patients and feedback to the community will also strengthen health promotion and community mobilisation for other trachoma elimination activities – mass drug administration and interventions for facial cleanliness and environmental improvement.
Managing post-operative trichiasis
Individual patients should be advised by the surgical team that trichiasis can return after surgery, especially in patients who had severe trichiasis before the operation. Patients should be told to seek medical help if they develop symptoms of trichiasis again. When a patient does seek help, someone familiar with treating post-operative trichiasis should assess them.
Trichiasis surgeons should carefully assess all patients found to have post-operative trichiasis and determine whether or not they need additional treatment.
- If the trichiasis is mild, with only a few lashes touching the peripheral parts of the eye, epilation can be considered
- If the lashes are central and regularly coming into contact with the cornea, then repeat surgery may be needed. Ideally the patient should be assessed by an ophthalmologist or by the most experienced trichiasis surgeon available.
The type of procedure surgeons use to correct the post-operative trichiasis will depend on the anatomical abnormality. It may not be appropriate to simply repeat the same operation that was undertaken for the primary trichiasis. The eyelid may have been shortened slightly by the original surgery. In these cases, a procedure which lengthens the eyelid may be needed to ensure good eyelid closure and protection of the eye.
Trachoma programme managers should monitor data on post-operative trichiasis for each outreach campaign and for individual surgeons. They should use the data, in collaboration with surgeons and their supervisors, to help actively manage trichiasis surgical outcomes.
Every manager needs to have a system for detecting and managing post-operative trichiasis:
- Patients should be followed up and assessed for post-operative trichiasis at least 6 months after surgery
- Surgical outcome must be recorded; follow-up data on any post-operative trichiasis should also be systematically collected and collated. For quality assurance purposes, these data should ideally be analysed for each surgeon.
If a surgeon is found to have an unusually high post-operative trichiasis rate (e.g., 30% at 6 months after surgery) then enhanced supportive supervision by a more experienced surgeon, or re-training, may be needed.
The role of national trachoma programmes in managing post-operative trichiasis is to:
- Monitor surgical outcomes, including data on the appearance of eyelids and recurrence of trichiasis after surgery, across districts
- Assess whether rates of post-operative trichiasis are affecting acceptance of surgery in the community. To do this, programmes need to put quality assurance systems in place to track data. Trends on post-operative trichiasis rates at the 6-month follow-up can be used as a measure of quality.
Data collection for monitoring trichiasis surgery
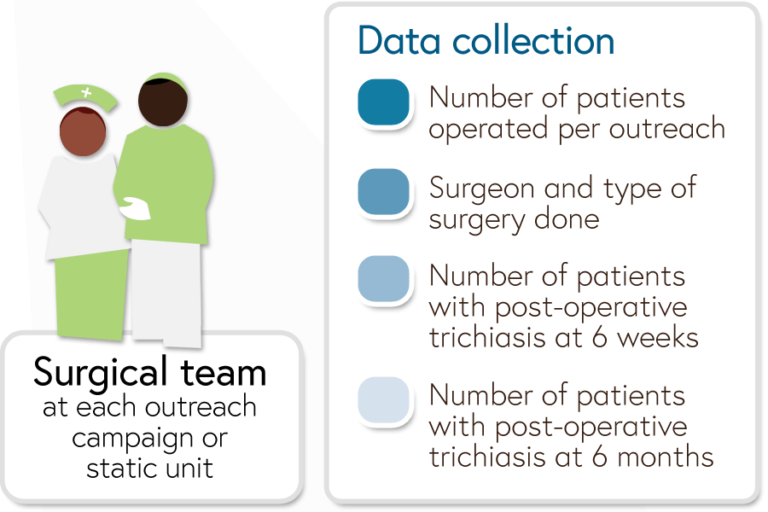
At each outreach campaign or static unit the following information on trichiasis surgery should be collected by the team:
- Number of patients operated per outreach
- Surgeon and type of surgery done
- Number of patients with post-operative trichiasis at 6 weeks
- Number of patients with post-operative trichiasis at 6 months
Share this

Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free








