Prevention is better than cure
Earlier this week, you learnt about how antibiotics work, how pathogens gain antimicrobial resistance (AMR) and how they spread resistance genes via horizontal gene transfer (HGT). We urgently need new antimicrobials, but the development of new pharmaceuticals is a very expensive task and there is no guarantee of success. It often takes many years of extensive testing, initially in the laboratory and later in clinical trials, before a new antimicrobial can be used clinically. When a new antimicrobial is developed, we now understand that we need to limit its use to try to reduce the risk that pathogens will evolve resistance to the new drug. This doesn’t sound like a great financial incentive for a pharmaceutical company to make a huge investment in the development of a new antibiotic!
An alternative strategy is to prevent infections from happening in the first place. There are several ways to do this, including public sanitation measures (eg sewage treatment, access to clean drinking water), personal hygiene (eg hand washing), controlling insect vectors (eg mosquito nets, insecticides, biocontrol) and vaccination programmes. In this Step, you’ll explore how vaccines work and how different types of vaccines are produced.
How do vaccines work?
Vaccines work by imitating particular chemical features (called antigens) that are found in a species or strain of pathogen, and activating an immune response in which your body produces white blood cells, called memory B-cells and memory T-cells. If the pathogen tries to infect you after you have been vaccinated, the T cells will recognise the specific antigens and activate memory B-cells to produce antibodies, proteins that bind to antigens. The antibodies bind to antigens (Figure 1). The antibodies bind to the antigens on the surface of the pathogen and help the immune system to neutralise or destroy it before it can establish an infection.
Figure 1: Schematic diagram of an antibody and antigens © Fvasconcellos [Public domain]
How are vaccines produced?
The majority of vaccines that are currently available fall into four main categories:
-
Live-attenuated vaccines are weakened versions of the pathogen that are able to replicate but do not cause disease symptoms. This type of vaccine tends to give very good protection, but they cannot be given to people with a weakened immune system (eg the young and elderly or those undertaking chemotherapy).
-
Inactivated vaccines contain whole pathogens, which have been treated with chemicals, heat or radiation so that they are no longer able to replicate. The immune response to this type of vaccine is often not the same as the real pathogen so several doses are often needed to build sufficient immunity.
-
Subunit vaccines contain the antigenic parts of the pathogen (typically polysaccharides or proteins usually found on the outside of the pathogen), which induce the immune response. They can be made by purifying specific parts of the whole pathogen or using cloning techniques to produce recombinant proteins (you’ll find out more about this later this week).
-
Toxoid vaccines are a specialised type of subunit vaccine containing inactivated bacterial toxins which are effective in cases where the toxin is the main cause of illness.
You can see some examples of the vaccines in current use in Table 1.
| Live-attenuated | Inactivated | Subunit | Toxoid |
|---|---|---|---|
| Polio (oral) | Polio | Pneumococcal disease | Diphtheria |
| Rotavirus | Rabies | Meningococcal disease | Tetanus |
| Chickenpox | Hepatitis A | Haemophilus influenzae type b: the HiB vaccine | |
| MMR: Measles, Mumps, Rubella | Whooping cough | Whooping cough: the acellular pertussis vaccine | |
| Influenza (nasal) | Influenza | Influenza | |
| Yellow fever | Japanese encephalitis | Human papillomavirus; the HPV vaccine | |
| Typhoid (oral) | Typhoid | Hepatitis B; the HBV vaccine |
Table 1: Examples of current vaccines. Note: vaccines are administered by injection unless alternative stated in brackets.
Eradication through vaccination
Much progress has been made over the last century in reducing the number of cases of infectious diseases through sanitation and vaccination programs, but there is still a long way to go. The last natural case of smallpox occurred in 1977, and in 1980 the WHO declared it to be eradicated. It remains the only human disease to have been successfully eradicated through mass vaccination programmes (Figure 2). The Global Polio Eradication Initiative (GPEI) is working hard to put an end to the devastating disease Poliomyelitis, which can cause paralysis and death. You can read more about the efforts of the GPEI to rid the world of Polio here.
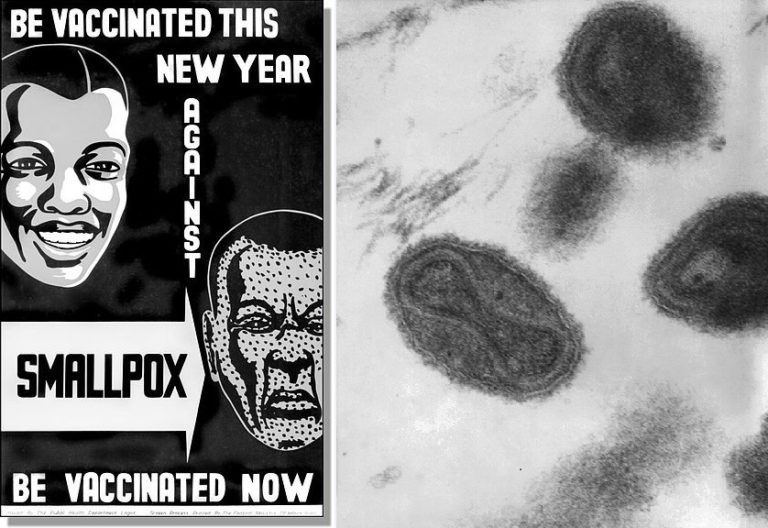

Figure 2: Top left: Poster produced during smallpox eradication campaign © Centres for Disease Control and Prevention [public domain]. Top right: Transmission electron microscope (TEM) image of the smallpox virus, now eradicated from the world © CDC/ Dr. Fred Murphy; Sylvia Whitfield [public domain]. Bottom left: A smallpox vaccination kit © Centres for Disease Control and Prevention [public domain]. Bottom right: Close-up of smallpox rash on child’s arm, photographed in Bangladesh in 1973 © Centres for Disease Control and Prevention [public domain]
There is growing concern that false claims of so-called “anti-vaxers” on social media and the internet has led to decreased take-up of childhood vaccinations, meaning potentially fatal and life-changing diseases like measles are causing serious outbreaks. In fact, the WHO have published their top ten list of global threats to human health, and vaccine hesitancy appears on this list. Work is being done to address these concerns, such as this guide from the Centres for Disease Control and Prevention (CDC) which answers frequently asked questions from parents about vaccines.
What else should governments to do encourage vaccination uptake? Have you heard of any news stories about this?
Recommended reading
-
Historical vaccine development and introduction of routine vaccine programmes in the UK timeline Public Health England
-
Vaccines and alternative approaches: Reducing our dependence on antimicrobials
Share this
Small and Mighty: Introduction to Microbiology

Small and Mighty: Introduction to Microbiology


Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free







