Occupational Health: What Are the Common Risk Factors?

Share this step
The field of Occupational Health covers a wide area. We hope you will find it interesting. It should be included in public health programmes in all countries. Industry is increasing in developing countries, and knowledge about occupational health is necessary to reduce health problems related to this activity.
When you work with “Occupational health”, your task is to avoid and reduce the effect of factors in the work places which may cause any adverse health effects among the workers. To have a work place and earn your salary, is of course a very important issue, but nevertheless, factors at work can sometimes have unwanted side effects. In occupational health we try to reduce these side effects. We aim to obtain good health among the workers. As one industrial leader once said to me: We should produce goods, not patients! In occupational health this is the main task: To avoid workers becoming patients. Some examples of work situations where risk factors for health appear will be described for you. Hopefully, the examples will give you a better understanding of what occupational health is. Along with the examples themselves, the difference between acute and chronic health effects will be explained to you.
a) Acute health effects
Example 1
My first example is regarding work in a saw mill.

A saw mill. © Colourbox
Here the workers cut timber to get materials ready for building purposes. However, there are dangerous tools such as saws present in this working environment.
A saw can be very dangerous. © G. Tjalvin
The workers cut the timber, but can also cut other things, for example, the hands of the worker. Our –yours and mine – awareness is now increased regarding possible risk factors for adverse health effects when working in saw mills by looking at these photos. However, we can do several things to avoid such injuries from happening. That is what occupational health is about.
Enclosed saw blade. © G. Tjalvin
On the photos you can see that we can enclose the moving part of the saw so the worker does not come in contact with the saw blade easily. We can also have security systems, so the saw blade is not turning if the saw is not well enclosed, and the saw can be in a special place or special room where no one other than the saw technician is located.
 Enclosed saw blade and worker with gloves. © Colourbox
Enclosed saw blade and worker with gloves. © Colourbox
We can also protect the worker, for instance by giving them strong, protective gloves, but for this particular case, strong gloves are not at all as good as the technical installations and enclosure I described. Anyway, I think you might get the point: We can prevent these accidents.
Example 2
There are many other potential risk factors at different work places. Another example is that health personnel may develop infectious diseases during contact with patients with such diseases. A very serious example is the Ebola outbreaks. Ebola is a deadly disease where we have little treatment to offer our patients. During the Ebola outbreaks in 2014-2015, the World Health Organization (WHO) reported a large number of deaths among health personnel. This is summarised in a report about the impact of the Ebola epidemic on the health workforce of Guinea, Liberia and Sierra Leone, covering the period from 1th January 2014 to 3th March 2015. Later, we have seen several new outbreaks, especially in DrCongo. The last report from DrC came in March 2020. Ebola is far more dangerous than for instance the Coronavirus we face in 2020, since it often causes deaths. However, the Coronavirus might be a huge problem as well, if it ends up with a pandemic, affecting very many persons -including many health personell.
815 health personnel died
due to confirmed/probable
Ebola disease in the period
from January 2014 to March 2015.
 Personal protective equipment for health personnel involved in the care of a Ebola patient: Powered air purifying respirator and full body suit ©Oslo University Hospital, Anders Bayer
Personal protective equipment for health personnel involved in the care of a Ebola patient: Powered air purifying respirator and full body suit ©Oslo University Hospital, Anders Bayer
However, such infections among health personnel can be prevented. This photo shows the protective equipment for health personnel working with an Ebola patient, and organizing her bed. They are using whole body suit with integrated helmet, each suit equipped with a powered air purifying unit creating positive air pressure within the suit. This equipment protects the health personnel from being exposed to the virus. Correct use of protective equipment will reduce the Ebola risk among the health personnel. Here we show the optimal protective equipment for such situations.
Example 3
 Rose farm with large numbers of green houses. © B.E. Moen
Rose farm with large numbers of green houses. © B.E. Moen
The third example is from East Africa. There are an increasing number of flower farms here, especially farms growing roses. Roses are very popular in the Western world, and large numbers of roses are exported from several countries in East Africa, such as Tanzania, Ethiopia and Uganda. These flower farms are huge, like you see in the photo, with many greenhouses. The farms employ thousands of people.
 Roses stored after cutting in a green house. © K. Segadal
Roses stored after cutting in a green house. © K. Segadal
The roses from the farms are transported to other countries. They are sent from the farms first by trucks and then by airplane every day, so the roses are fresh when they arrive.
Last year, a truck filled with roses at a flower farm was ready to travel to the airport with the roses at the end of the day. One leader at the flower farm passed by, observing that some space was not filled up in this truck. He asked two women working there, to cut more roses from the green house, to fill in this space. There was not much time before the plane should leave, and things had to be done quickly. The women protested, because the green houses where the roses were growing had just been sprayed with pesticides, and no one should enter.
 Cutting roses in a green house. © K. Segadal
Cutting roses in a green house. © K. Segadal
Normal practice is that the pesticide sprayers close up green houses some hours after spraying, to avoid human exposure to these toxic substances. In this case, the female workers were not listened to, but told to be quick, to go into the green house and cut more roses. They did so. Immediately afterwards, they felt very sick, with nausea, headache and vomiting. One of the women died the same day; she had serious pesticide intoxication and her kidneys stopped working.
This is a tragic example of an avoidable situation. The workers should not have entered the green house just after spraying. There are strict rules about waiting a certain amount of time after spraying before re-entering the area, to avoid workers running the risk of inhaling these substances. Or – if the workers need to enter, they should be equipped with personal respiratory protective equipment so they do not inhale or get in contact with the toxic pesticides.
b) Chronic diseases at work
The types of risk factors described in the examples so far cause acute health effects, meaning they develop at the time of exposure at work or soon after. In working life, however, workers may also be exposed to factors that cause adverse health effects over longer periods of time. In occupational health we call these chronic diseases. One such factor is dust. Dust can be inhaled and reach the lungs and cause respiratory problems. Sometimes, these types of lung diseases do not develop until after years of exposure. This is the situation for coal miners for instance, like the ones you see in the photo. Inhaling coal dust over years may cause coal miners’ pneumoconiosis, a disease which at first will cause cough during work in this dust. At first this symptom may be considered as an acute health effect; the dust irritates the air ways. However, after some time, the cough may worsen and in addition serious problems in breathing may develop. This is a typical start of the pneumoconiosis; a chronic disease that we cannot cure. Workers with this disease may become invalided and unable to perform any further work. However, this is a disease we can prevent. If you are skilled in occupational health, you will know, for instance, that using water during drilling will reduce the dust in the air, and also that respiratory protective equipment exists, which can reduce the amount of dust exposure for the worker.
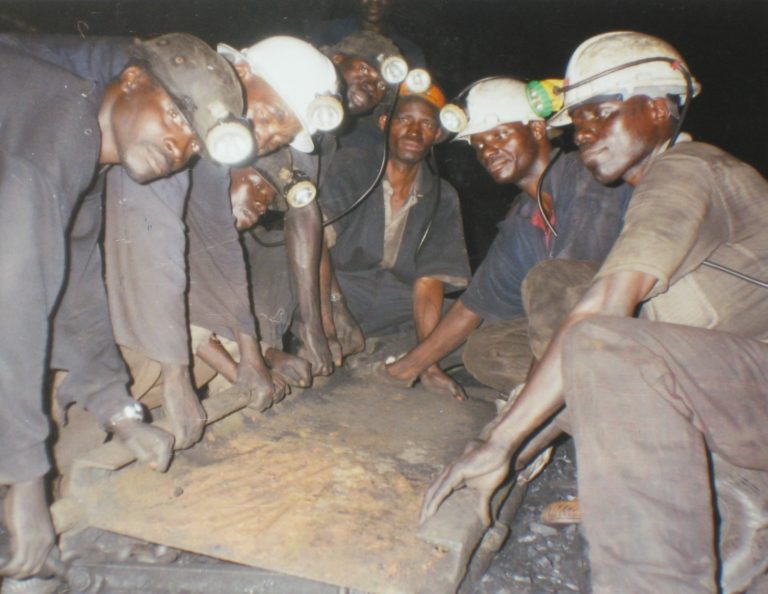 Coal miners from Tanzania. © S.H.D. Mamuya
Coal miners from Tanzania. © S.H.D. Mamuya
Share this
Occupational Health in Developing Countries

Occupational Health in Developing Countries


Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free







