Patient pathway: Mary’s story
The pathway to radiation therapy can be different for each person. However, most people follow a similar route. Listen to Mary’s fictional story by clicking on the audio button beneath each picture, and learn about her pathway from diagnosis to survivorship.
You will hear Mary’s thoughts on her treatment for breast cancer, and the voices of her healthcare team who helped deliver her radiation therapy.
Once a month, Mary set a time each day to check her breasts for anything unusual. This was done routinely and no changes were found except for today.
Mary noticed that there was a little lump there that was not present before. This made her very anxious and concerned. At first she hoped it would go away.
She checked again and it was still there; it was time to get it checked. She booked an appointment to go and see her doctor.
 Visit to General Practitioner or Family Doctor
Visit to General Practitioner or Family Doctor
The doctor met with Mary and did a full physical examination of her. The doctor also felt the lump and explained to Mary that it was important for her to go and get this checked further with some specialist tests.
The doctor sat Mary down and explained clearly what would happen next. Mary was very worried, however she was happy that she went to see the doctor.
Mary received an appointment in the post to go to the hospital for further checks. At the hospital she had a triple assessment.
- She had a mammogram. Her breasts were put in between two x-ray plates and images were taken from several angles. This hurt a little as her breasts had to be flattened however it was manageable and bearable and not as bad as she had imagined it to be.
- She then had an ultrasound and a breast biopsy. The doctor took a sample of tissue from the breast and sent it away to be analysed in the laboratory.
The biopsy would confirm if the tissue in the lump was cancerous or not.
When the results were returned, Mary was asked to come into the doctor’s office to discuss them.
She was told she had breast cancer and that she would need treatment.
- Her first treatment was surgery. During surgery the doctor removed the lump and some surrounding tissue (lumpectomy) to ensure that all the cancer was removed. She did not need to have her entire breast removed (known as a mastectomy).
- She was referred to a social worker who could advise her on financial matters. She was also made aware of support groups that could help her and her family.
- After surgery she received chemotherapy (known as adjuvant treatment) for several weeks before her radiation therapy began. Some chemotherapy drugs can cause hair loss and this happened in Mary’s case.
- In addition to this she also was prescribed hormone therapy and HER2 targeted drugs. These are used when a cancer is HER2 positive and hormone receptor positive.
 Radiation Oncology Referral CT Scan
Radiation Oncology Referral CT Scan
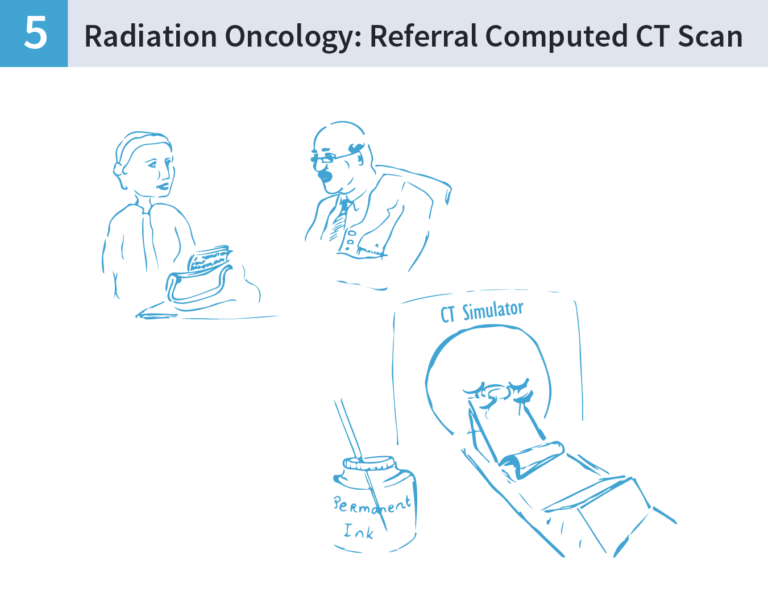
When her surgical site was healed and her chemotherapy finished, Mary was sent to a radiation therapy department to receive the remainder of her treatment. Her first appointment was with the radiation oncologist who explained what radiation therapy is and the side effects from it. Mary gave informed consent to begin this treatment.
To get her treatment planned Mary went to the radiation therapy department with her husband. She was called from the waiting room into the Computed Tomography (CT) scanning room.
- In this room she was asked by the radiation therapist to lie down on special equipment (breast board) to help get her into the correct position. The breast board helped hold her arms over her head.
- She found this difficult however the radiation therapists were very kind and helped her into position. She had to remove all of her top clothing before getting onto the couch, but she was given a gown to cover herself until she was on the couch.
- Once on the couch she was put into the correct position for treatment and scanned. When the scan was completed she had three permanent tattoos placed on her skin. At first she did not want these, as she was afraid that they would be painful and unsightly. However when she realised that they were not painful and only the same size as a freckle, she did not mind. The tattoos are used by the radiation therapists to position Mary daily.
- The images taken in the CT were sent to the doctor and the planners who decided exactly how much dose Mary would get. This was a plan made specifically for Mary.
 Radiation Therapy on Linear Accelerator
Radiation Therapy on Linear Accelerator
After about two weeks Mary started her 3 weeks of treatment. She was very nervous about treatment and was worried that it might hurt her. She met with the radiation therapists on the first day and they explained in detail what was going to happen. This put her at ease and she built a good rapport with the radiation therapist. She saw mostly the same professionals daily and liked discussing any concerns she had with them.
 Daily Treatment and Side Effect Management
Daily Treatment and Side Effect Management
After the second week, Mary noticed that her skin got slightly red. She mentioned this to the radiation therapists who advised her on how to manage the skin reaction. During treatment she also got to meet the doctor again. She liked the support she got from the hospital multi-disciplinary team; the radiation oncology nurse, radiation oncologist and radiation therapist. There was always someone to answer her questions.
When Mary finished treatment the radiation therapists informed her that even though she has finished radiation therapy, it will keep on working for at least another 10 days before it reaches its peak reaction.
Radiation therapy keeps on working even if your treatment is finished: this is referred to as the cumulative effect.
During this time Mary found that her skin reaction became more pronounced than during treatment. This worried her however the radiation therapists explained that this was a normal side effect for breast radiation therapy and would get better over time. The radiation therapist gave her the unit number so she could call if she had any further worries.
After treatment had finished, Mary received an appointment informing her that she had a follow up appointment in 6 weeks’ time to see how she was managing. Mary was told that she will be monitored for the next five years.
- At first checkups are every three months, then six months, then annually.
Mary was told if she had any worries, concerns or problems between these times to contact the doctor again.
In the comments section below:
Think about the story you have just heard and share your answers to the questions below in the comments section.
- What is Mary thinking and feeling during the start and end of her pathway? And why?
- How would you react if you were Mary?
- How would you react if you were a friend of Mary’s?
You can download the full podcast of this story here
To download:
- Right-click on “here” above and select “Open in a new tab”. The audio will begin playing in a different tab.
- Click the three dots on the right and then select “Download”. The audio file will now begin downloading.
Image credits: Meadhbh Arthurs
Share this
An Introduction to Radiation Oncology: From Diagnosis to Survivorship

An Introduction to Radiation Oncology: From Diagnosis to Survivorship


Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free