Home / Healthcare & Medicine / Cancer / An Introduction to Radiation Oncology: From Diagnosis to Survivorship / Setting the scene: Pre treatment
This article is from the free online
An Introduction to Radiation Oncology: From Diagnosis to Survivorship


Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.

 Clinic room
Clinic room
 CT Scanner
CT Scanner
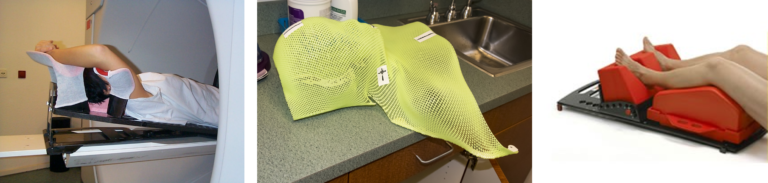 L to R: Immobilisation devices – Breast board, mask, knee/foot fix
L to R: Immobilisation devices – Breast board, mask, knee/foot fix
 MRI Scanner (stock photo)
MRI Scanner (stock photo)
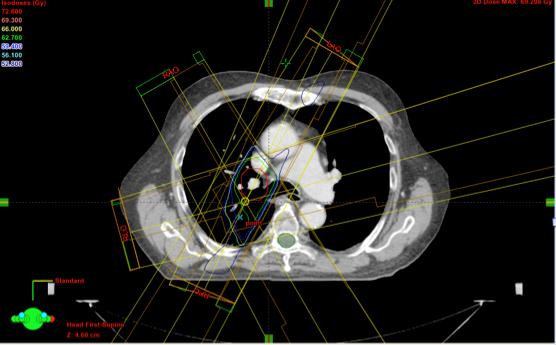 This is a treatment plan for a lung cancer patient. The tumour or target is delineated in red. The spinal cord, which is an organ at risk, is delineated in green.
This is a treatment plan for a lung cancer patient. The tumour or target is delineated in red. The spinal cord, which is an organ at risk, is delineated in green.






