The RSI Kit Dump

Share this step
In the step Lara Hammond (KSS HEMS Paramedic) and Julian Wijesuriya (KSS HEMS Doctor) describe the principles and practice of setting up a standardised RSI kit dump for pre-hospital emergency anaesthesia and intubation.
Introduction
The ideal location for anaesthesia and airway management is the hospital anaesthetic room, which gives clinicians a safe, well-organised space to work. There are many essential components to the anaesthetic room setup that can easily be taken for granted. Pre-hospital scenes, by definition, do not offer such “luxuries” and present a number of additional challenges. It is incumbent on pre-hospital clinicians to create a safe space containing these essential components before undertaking pre-hospital emergency anaesthesia.
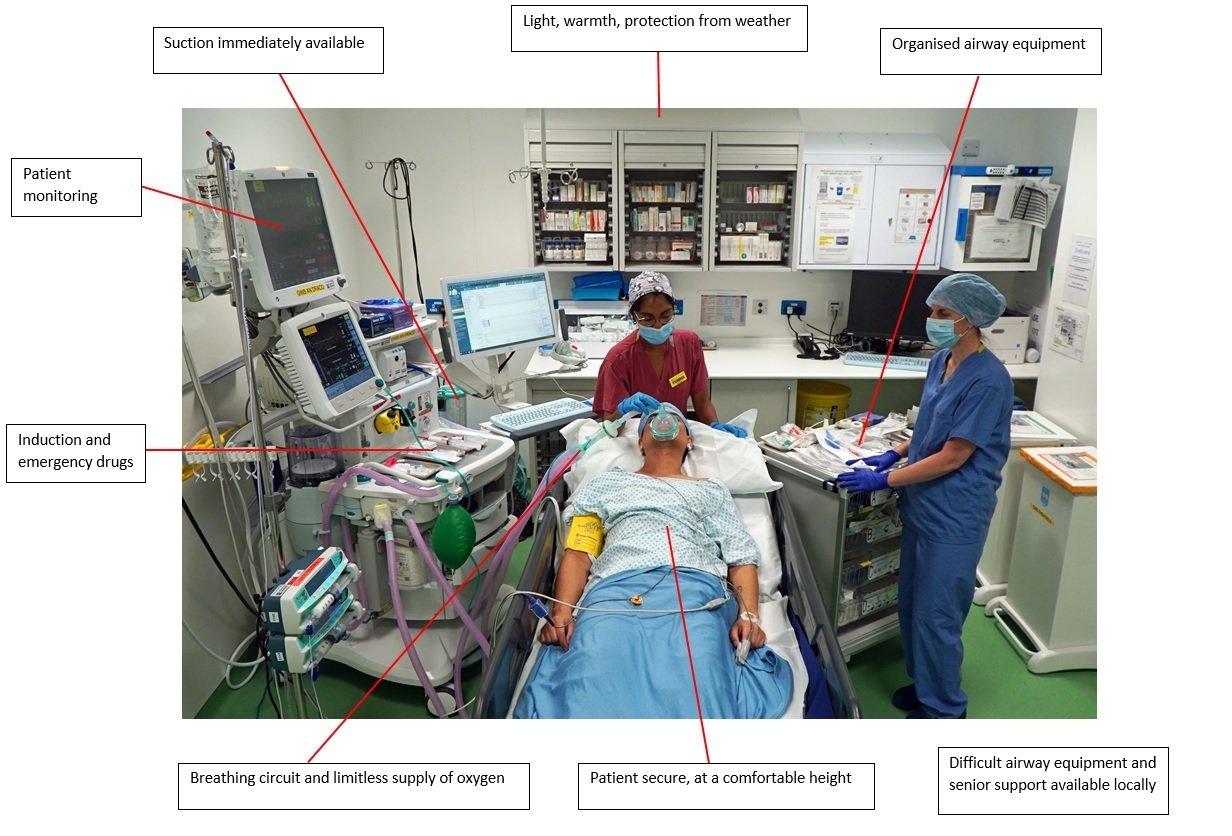 Components of a hospital anaesthetic room
Components of a hospital anaesthetic room
The RSI Kit Dump Concept
Safe pre-hospital anaesthesia and intubation requires a standardised setup that can be deployed on scene, comprising the required personnel, equipment and environmental protection. This is colloquially termed “the RSI kit dump” and is established by the airway assistant. However, the term is somewhat of a misnomer, as unlike its fairly simplistic name, there is a lot more to the RSI kit dump than may initially be apparent.
Every pre-hospital scene is different and it takes experience and skill to assess the scene, mitigate hazards and utilise available resources in order to rapidly establish an RSI kit dump.
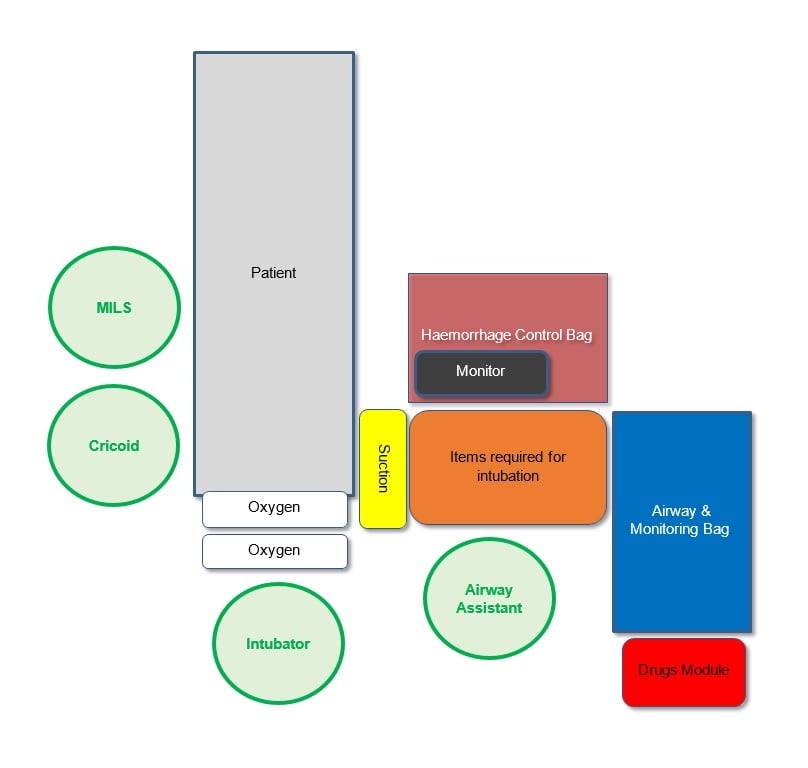 Schematic of a standardised RSI kit dump. Credit: KSS Standard Operating Procedures
Schematic of a standardised RSI kit dump. Credit: KSS Standard Operating ProceduresThe patient should concurrently assessed, treated and packaged in a standardised way, as you learnt in a previous step. This ensures that they are clinically stabilised, appropriately monitored, physically secure and in an appropriate position prior to induction of anaesthesia.
Selecting and Optimising the RSI Kit Dump Location
- Hazards
- Space & patient access
- Light, weather & terrain
- Noise
- Vehicle access & egress
- Patient privacy
- On scene resources
- Patient specific factors
Hazards
Space & Patient Access
Terrain & Weather
Light
Noise
Vehicle access & egress
Patient Privacy
Extreme Conditions
Practicalities & Setup
Airway Equipment Sheet
- RSI checklist and drug aide memoire
- Laryngoscope with chosen blade
- Appropriate ET tube with KY gel, 10ml syringe and tube tie
- Bougie or stylet
- Circuit including: inline ETCO2 monitoring, HME filter and catheter mount
- Temperature probe
- In-line suction
- Pre-drawn anaesthetic drugs
Equipment should be taken out of its packaging, checked and kept clean. In addition, secondary equipment such as supraglottic airway devices, surgical airway equipment and alternative laryngoscope blades should be prepared or close to hand if not laid out.
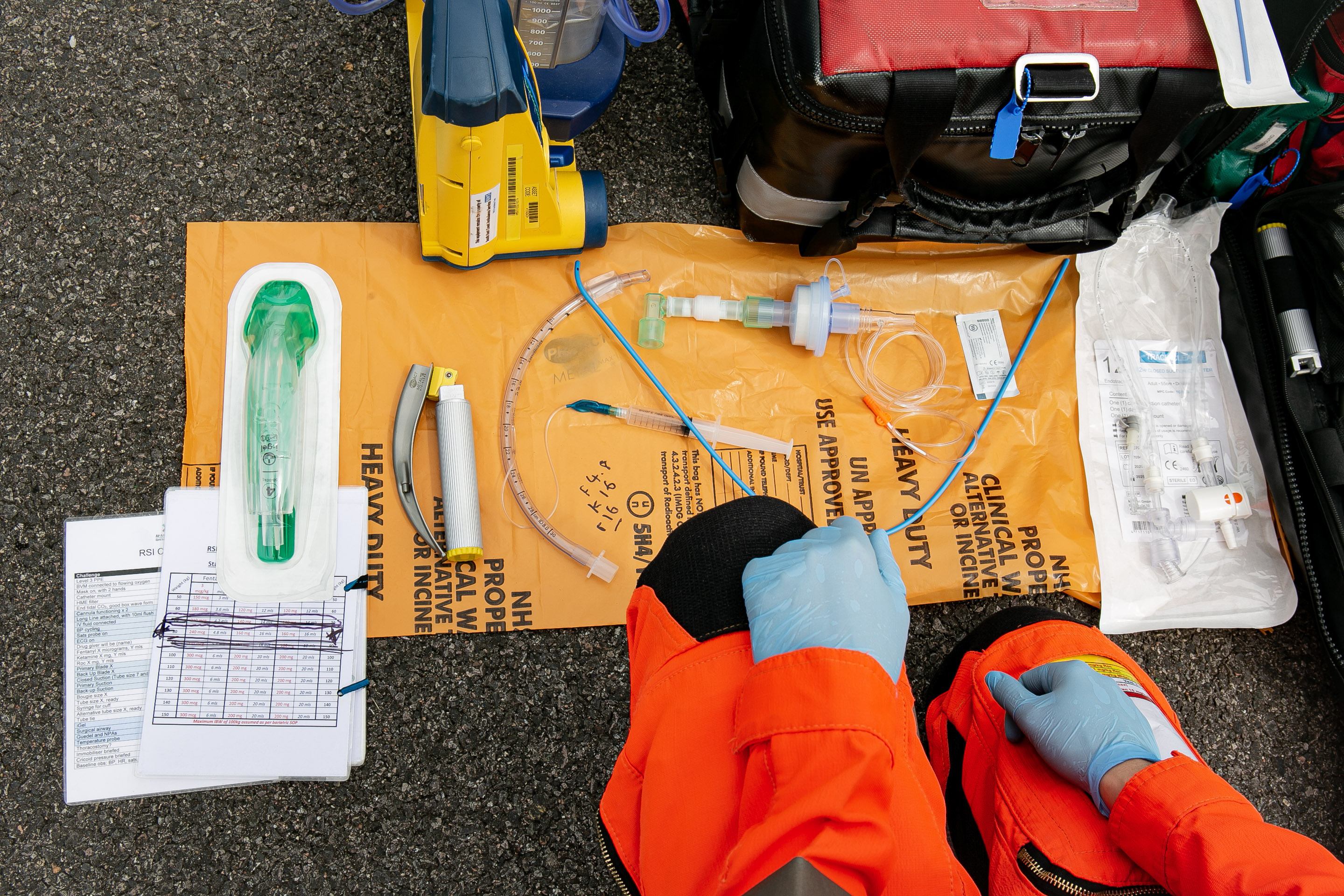 The airway equipment sheet (drugs not shown)
The airway equipment sheet (drugs not shown)
Additional Equipment
In addition, the following equipment is required:
- Two oxygen cylinders (confirmed full and with master valves open)
- Primary and backup suction units
- Emergency drugs
- Bag-valve-mask (BVM)
- Patient monitor
Some of this equipment may be with the patient and does not need to be duplicated. The figure below shows an overview of a prepared RSI kit dump prior to the patient’s arrival.
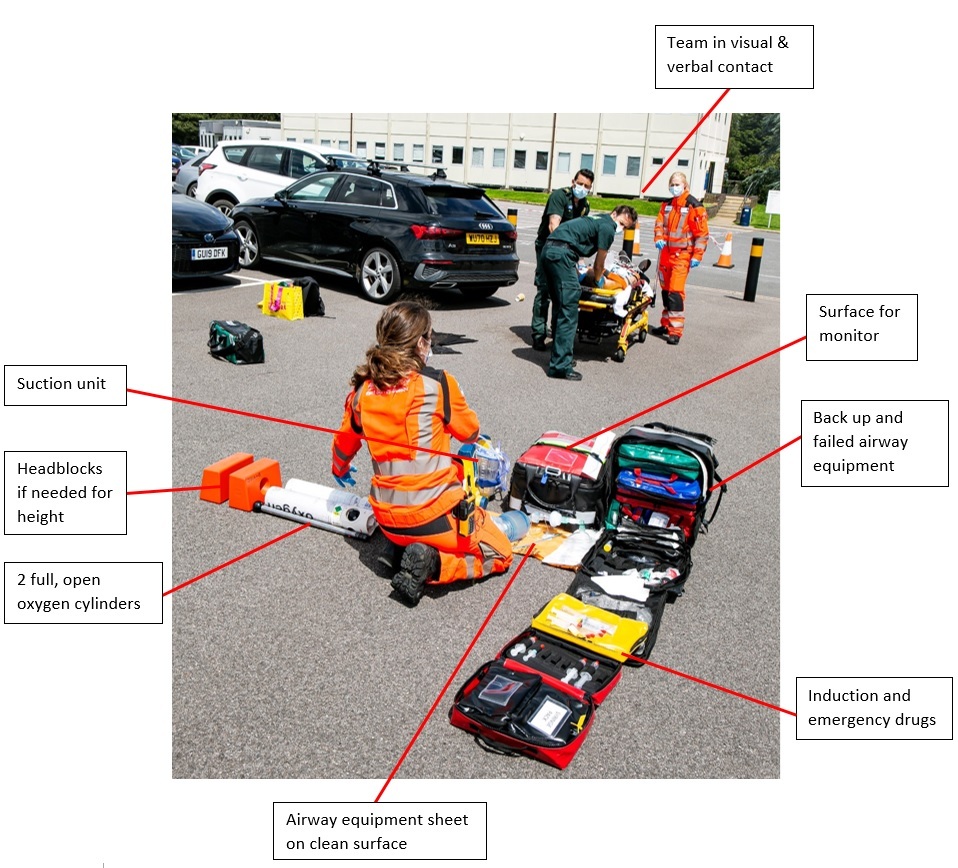 Overview of the RSI kit dump
Overview of the RSI kit dump
Objective
The ultimate goal is to achieve a safe, appropriately lit area that is flat, protected from the elements and allows full access to the patient. All the essential components of the hospital anaesthetic room should be present and organised in a standardised manner. In this setup the doctor and paramedic are side by side and at same level ensuring good communication, a shared overview, and in close contact for handling airway equipment.
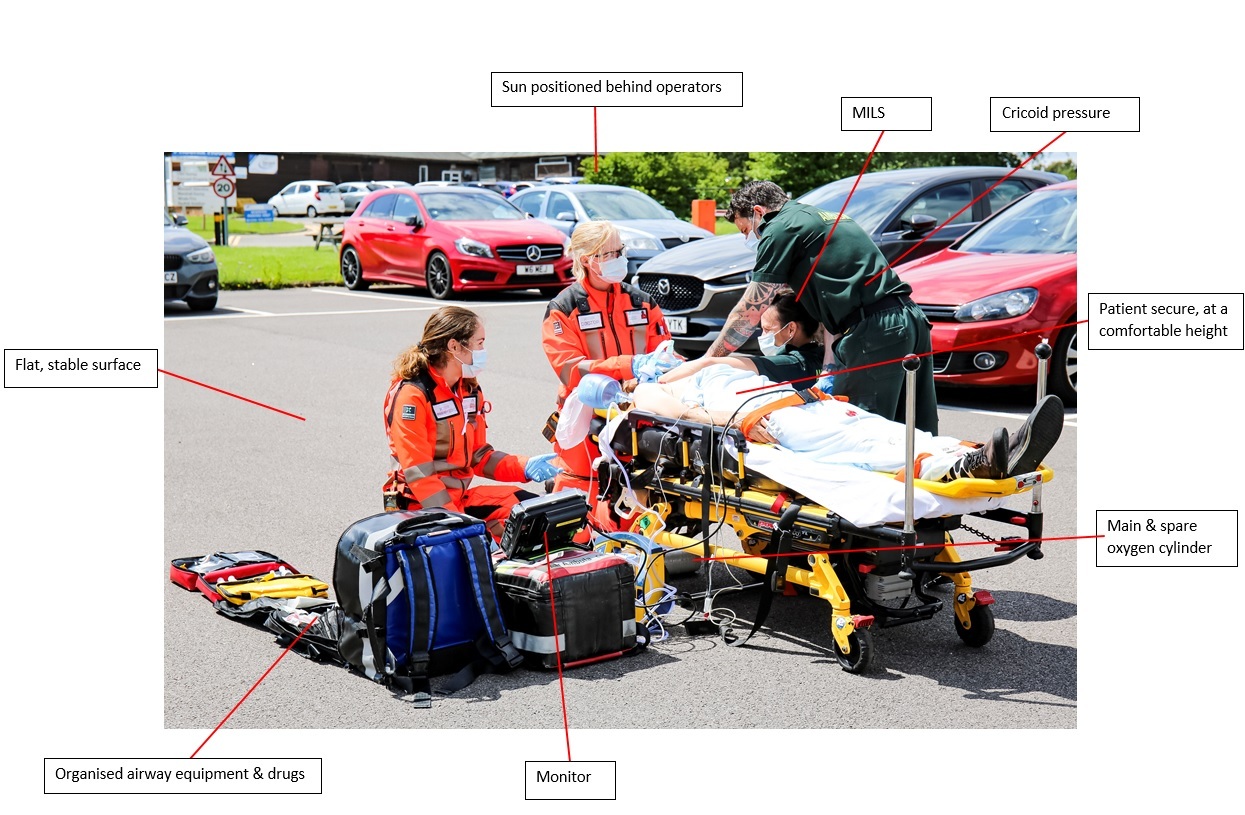 Complete RSI kit dump with patient and essential personnel
Complete RSI kit dump with patient and essential personnel
Team Dynamics
Initial Assessment
Two person pre-hospital teams should work together during initial patient assessment and management, with the general guideline to remain together “until the scoop is clipped” or in some cases until the patient is fully packaged. This ensures both team members have a shared understanding of the patient’s condition and can jointly plan further patient management.
At an appropriate time, the airway assistant will move away from the patient and their colleague and start setting up the RSI kit dump. Prior to this there should usually be a short discussion within the team regarding drug regimens and dosages, blade type and ETT sizes.
Communication & Situational Awareness
Ideally when setting up the kit dump, the airway assistant should remain in visual and verbal contact with their colleague who has remained with the patient. This enables them to assist if there are any changes in the patient’s condition and ensures both team members maintain situational awareness. This is an additional consideration when selecting the RSI kit dump location.
There may be instances where this is not possible, for example when a patient is inside a property and the RSI is planned to take place outside. In such cases, the airway assistant could peel away as extrication starts, in order to minimise the time they are out of contact or intermittently regroup with their colleague if appropriate.
Standardisation & Safety
Having standard operating procedures (SOPs) and rehearsal ensure that individual team members have a consistent approach to scene and patient management and the RSI kit dump process. This allows colleagues who have not worked together before to work safely and efficiently together, but also ensures that the process causes minimal cognitive loading. When dealing with chaotic scenes or complex patients, these practices can provide a feeling of familiarity, stability and control and this allows teams to regroup and restore bandwidth. Similar principles apply to the conduct of anaesthesia and difficult or failed airway drills.
Summary
The RSI kit dump represents the pre-hospital re-creation of the hospital anaesthetic room. The process optimises patient and team safety, ensures that vital equipment is available and that personnel have the space to work. Having a standardised process reduces cognitive loading and brings structure to chaotic scenes. Overall, the RSI kit dump is one of the cornerstones of safe pre-hospital anaesthesia and intubation.
Share this

Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free








