Pre-Oxygenation

Share this step
In this step Ros Perring (Anaesthetic Registrar, UCLH) and Julian Wijesuriya (KSS HEMS Doctor) go into some more details regarding the physiological principles and practice of pre-oxygenation in the pre-hospital setting.
Physiological Principles
Functional Residual Capacity
The functional residual capacity (FRC), is the volume of gas in the lungs at the end of expiration during normal tidal breathing. In a normal sized adult, the FRC comprises ~2500mL of gas made up of 21% oxygen, 78% nitrogen and 1% other gases. Pre-oxygenation is the process of optimising body oxygen stores prior to a period of apnoea. This is primarily achieved by a patient breathing (or being ventilated with) 100% oxygen to denitrogenate the lungs and optimise of oxygen storage within the arterial, tissue and venous compartments. In optimal conditions pre-oxygenation can increase the time to desaturation during apnoea from under two minutes to up to eight minutes.
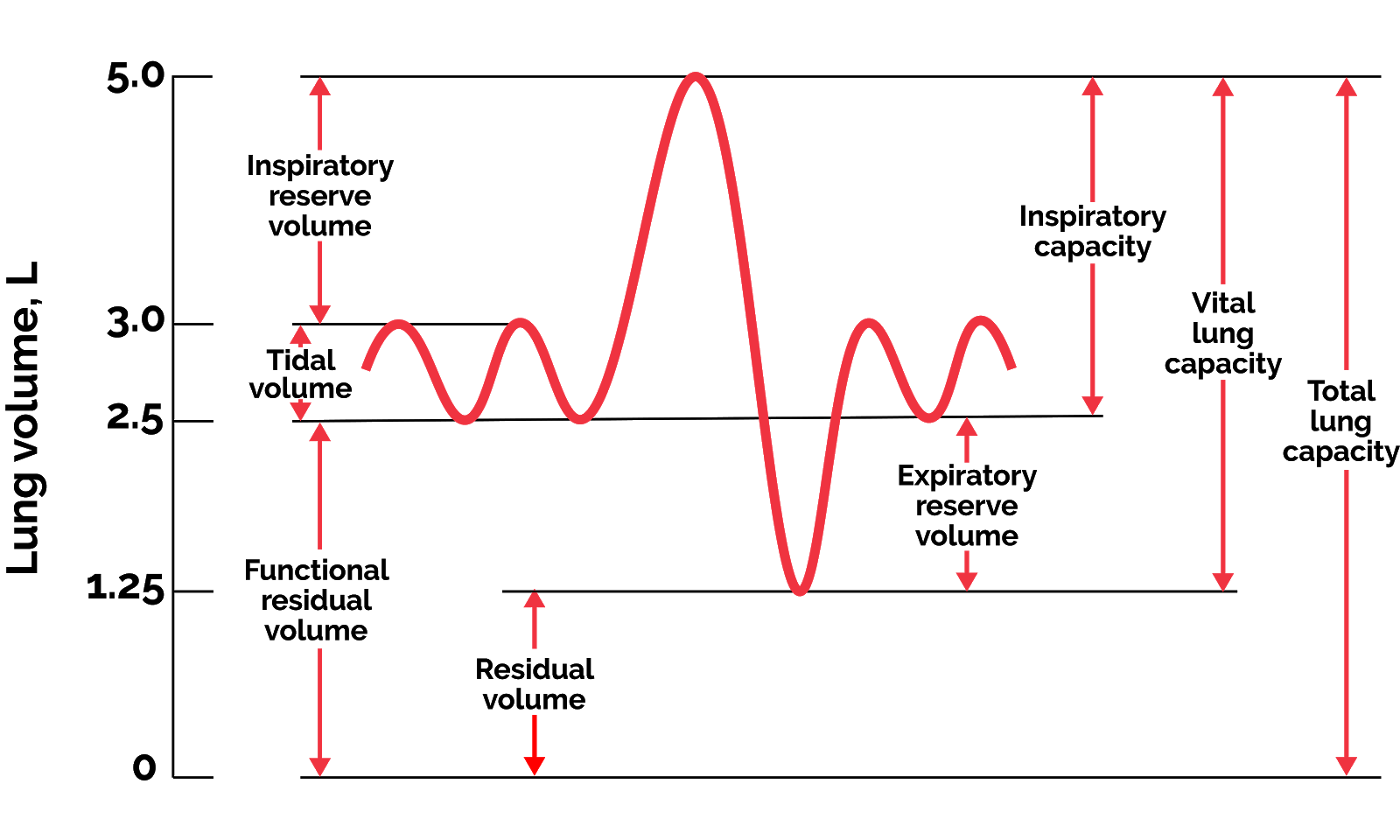 Lung volumes and capacities
Lung volumes and capacities
In a healthy person, the FRC is usually the point at which lung compliance is optimal, sitting on the steepest part of the lung compliance curve. This is the point at which it takes the smallest changes in pressure to generate changes in lung volume and where tidal breathing should normally occur. A lower FRC moves a patient to a less compliant part of the curve.
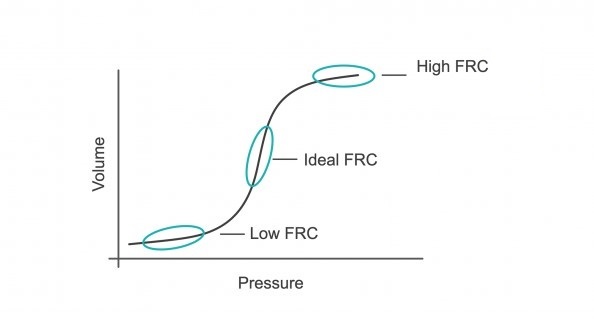 FRC and lung compliance
FRC and lung complianceClosing capacity and FRC
- Reduced oxygen stores – resulting in more rapid desaturation
- Reduced lung compliance – resulting in increased work of breathing or higher mechanical ventilatory pressures
- Increased intra-pulmonary shunt (the volume of blood passing through the lungs but not taking part in gas exchange) – leading to hypoxaemia
- Increased pulmonary vascular resistance – resulting in increased right ventricular afterload
The Efficacy and Efficiency of Pre-Oxygenation
The efficacy of pre-oxygenation describes the capacity to produce optimal end-tidal oxygen values (ETO2) through denitrogenation of the FRC. It is dependent on:
- Airway patency during pre-oxygenation and apnoea
- Fraction of inspired oxygen (FiO2)
- Fresh gas flow rate
- Duration of pre-oxygenation
- Type of breathing (vital capacity breaths vs. tidal breaths)
- Adequacy of the seal between the mask and the patient (Loss of the mask seal at any point during pre-oxygenation will result in a significant depletion of the oxygen reserve and replacement with nitrogen due to passive diffusion)
The efficiency of pre-oxygenation is represented by the rate at which desaturation occurs during apnoea. This is influenced by patient specific factors outlined below:
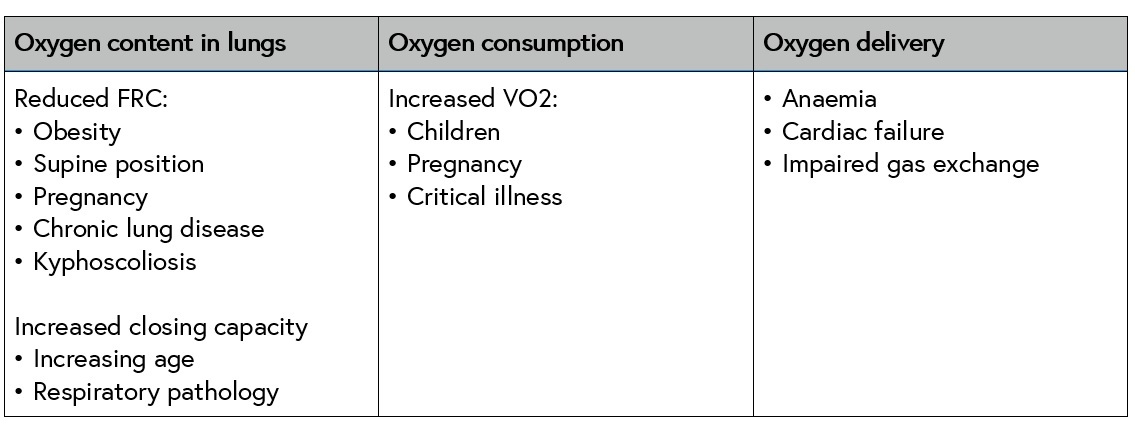 Factors affecting the efficiency of pre-oxygenation
Factors affecting the efficiency of pre-oxygenation
Many of these factors may not be modifiable, particularly in the critically ill or during emergency intubation. FRC can be optimised by applying PEEP during pre-oxygenation and keeping the patient as upright as possible.
Pre-Hospital Challenges
There are a number of a factors that can make it harder to achieve adequate pre-oxygenation in the pre-hospital setting:
- Patient pathophysiology: illness or injury resulting in cardio-respiratory compromise, neurological injury or major haemorrhage will impact the efficiency of pre-oxygenation by reducing FRC, impairing gas exchange, increasing oxygen consumption and affecting oxygen delivery. Some patients will desaturate within seconds despite pre-oxygenation attempts.
- Difficult airway: c-spine immobilisation or airway trauma causing haemorrhage or disrupted anatomy can make establishing airway patency and mask ventilation difficult, resulting in less efficacious pre-oxygenation.
- Patient positioning: in trauma patients spinal precautions necessitate flat supine positioning typically on a scoop stretcher or vacmat, this negatively affects FRC.
- Patient cooperation: confusion, agitation or combative behaviour may reduce the efficacy of pre-oxygenation through frequent breaks in face mask seal.
- Equipment: the gold standard for assessing the efficacy of pre-oxygenation is end-tidal oxygen (ETO2) monitoring. This monitoring is not routinely available in the pre-hospital setting and so clinicians have no objective indicator that they have achieved optimal pre-oxygenation prior to embarking on emergency anaesthesia.
Pre-Oxygenation Techniques and Optimisation Strategies
Pre-oxygenation techniques
Hospital-based techniques such as high-flow nasal oxygen, CPAP or NIV are typically not available pre-hospitally due to the bulkiness of equipment and rates of oxygen consumption. There are three main methods of pre-oxygenation in the pre-hospital setting: non-rebreathe (NRB) mask, bag-valve-mask (BVM) device and Mapleson C circuit – all of which have pros and cons.
NRB masks are often better tolerated in confused or agitated patients, however there is no option to deliver PEEP or manual ventilation and the FiO2 delivered is typically only 60-80%.
BVM devices allow delivery of near 100% FiO2, they facilitate the use of PEEP and basic ventilatory support and are robust devices. However internal valves increase the work of breathing in spontaneously breathing patients and they may be less well tolerated by patients.
Mapleson C circuits offer tactile feedback about a patient’s respiratory effort and lung compliance and they allow more nuanced delivery of PEEP and ventilatory support, however they are less robust than BVM devices and there is a greater risk of re-breathing and CO2 accumulation.
 Three methods of pre-oxygenation (L-R): Non-rebreathe mask, bag-valve-mask, Mapleson C circuit
Three methods of pre-oxygenation (L-R): Non-rebreathe mask, bag-valve-mask, Mapleson C circuit
Optimisation Strategies
Given the challenges of pre-hospital pre-oxygenation, close attention must be paid to adequacy of pre-oxygenation to avoid critical hypoxia following the induction of anaesthesia. It is possible to use the physiological principles already discussed to inform strategies that can optimise the process:
- Attention to detail:
- Ensure an adequate supply and delivery of high flow (15L/min) oxygen to the pre-oxygenation device
- Support airway patency with effective basic airway opening manoeuvres and airway adjuncts if tolerated
- Ensure a tight mask seal using a 2-handed 2-person technique. Information regarding seal quality can gained from the ETCO2 waveform
- Completing a full three minutes (tidal ventilation) of pre-oxygenation where practicable
- Where possible and appropriate pre-oxygenate with PEEP to optimise FRC, reduce airway collapse, improve lung compliance and reduce pulmonary vascular resistance.
- Patient positioning
- If circumstances allow, improve the patient’s body position by ramping the patient or raising the head of the trolley to improve FRC. Position the patient’s head and shoulders to achieve a “sniffing the morning air” position for optimal airway patency and ease of laryngoscopy
- In patients with maxillo-facial injuries or airway haemorrhage, pre-oxygenate and induce anaesthesia in the most comfortable position for the patient and that which minimises aspiration.
- Sedation
- In some cases of severe agitation it may be necessary to administer a pre-RSI sedative (such as ketamine) to gain control of the situation and facilitate adequate pre-oxygenation. This must be a carefully considered risk-benefit decision
- Oxygenation & ventilation during the apnoea phase
- In select patients (eg at high risk of rapid desaturation or difficult laryngoscopy) gentle ventilation during the apnoeic phase can delay time to desaturation. This must be balanced against the risk of gastric insufflation, regurgitation and aspiration
- Administration of O2 at 15 L/min via simple nasal cannulae supplements oxygen delivery for pre-oxygenation (eg in patients with high inspiratory flow rates or minute ventilation). This technique also provides degree of apnoeic oxygenation during laryngoscopy attempts and can delay time to desaturation.
Conclusions
Pre-oxygenation is a vital part of airway management in any setting. It is important to understand the underlying physiological principles and the practical considerations relevant to specific environments and patient groups. Optimising the efficacy and efficiency of pre-oxygenation, increases the safety profile of rapid sequence induction and maximizes the safe window available for laryngoscopy attempts and rescue strategies.
Share this

Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free








