Tips on Managing Diabetic Retinopathy Treatment

Share this step
As you read this article, consider why determining a patient’s ability to come for follow up is an important consideration when selecting the treatment approach.
This article is adapted from Hall A. (2011). Recognising and managing diabetic retinopathy. Comm Eye Health, 24(75), 05 – 09 and the International Council of Ophthalmology (2017) Guidelines for diabetic eye care.
ICO guidelines for diabetic eye care
1. Optimise medical treatment
- Improve glycaemic control if HbA1c > 58 mmol/mol (>7.5%) as well as associated systemic hypertension or dyslipidemia.
2. No diabetic retinopathy, mild or moderate non-proliferative diabetic retinopathy
- Follow at recommended intervals with dilated eye examinations and retinal imaging as needed
- Treat diabetic macular oedema as needed.
3. Severe non-proliferative diabetic retinopathy
- Follow closely for development of proliferative diabetic retinopathy in high resource settings
- Consider early panretinal photocoagulation for patients at high risk of progression to proliferative diabetic retinopathy or poor compliance with follow-up and in low-resource settings.
4. Proliferative diabetic retinopathy
- Treat with panretinal photocoagulation (PRP) or
- Anti-VEGF injections (ranibizumab) are a safe and effective treatment through at least 2 years, and other intravitreal anti-VEGF agents (aflibercept and bevacizumab) are also highly effective against retinal neovascularization.
Key learning points
- Diabetic retinopathy is treatable. Treatment usually maintains vision but does not restore vision that has already been lost
- For diabetic maculopathy, laser or anti-VEGF injections are both proven to work
- Proliferative retinopathy is best treated with pan-retinal laser. The commonest error is under treatment, and laser should be applied until there is regression of the new vessels or there is no room for further treatment
- Vitrectomy is useful for vitreous haemorrhage and late complications of proliferative retinopathy. Pre-treatment with bevacizumab reduces the risk of surgical complications.
Treating proliferative diabetic retinopathy
The two main treatment options for proliferative diabetic retinopathy are pan-retinal laser photocoagulation and diabetic vitrectomy.
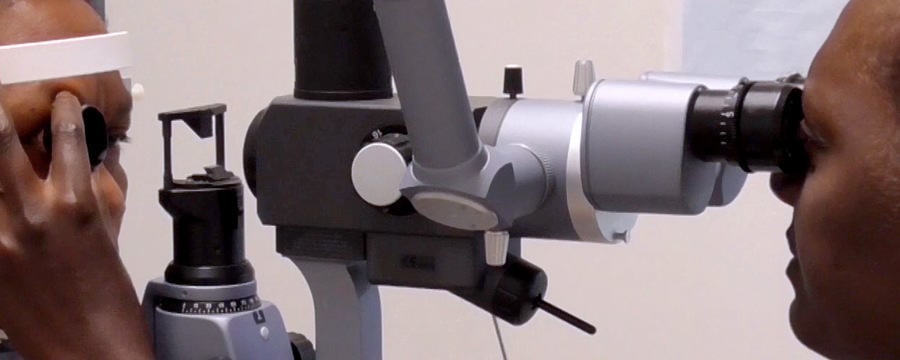
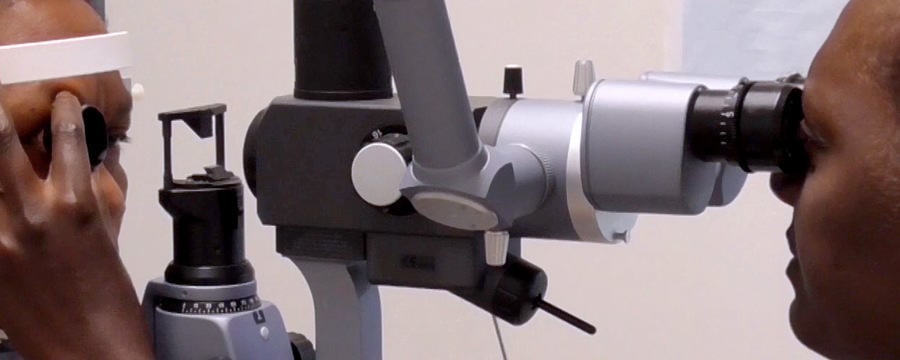
Pan-retinal photocoagulation (PRP)
PRP, or scatter laser, is the main form of treatment for proliferative diabetic retinopathy. The aim of the laser is to induce regression of new blood vessels (that is, to make them stop growing and shrink). The laser burns must be given early enough and cover enough retina to shrink the new blood vessels that cause the complications of vitreous haemorrhage and tractional (due to a pulling action) detachment of the retina.
A 50% reduction in severe visual loss after PRP was reported by the Diabetic Retinopathy Study for patients with new vessels on the optic disc (proliferative diabetic retinopathy).
Pre-treatment discussion with patients (ICO, 2017)
- Patients usually need numerous follow-up visits and may require supplementary laser treatment
- PRP reduces the risk of visual loss and blindness
- Laser treatment often reduces peripheral and night vision; treatment may moderately reduce central vision
- Although laser treatment is effective, some patients may still develop vitreous haemorrhage. The haemorrhage is caused by the diabetes and not by the laser; it may mean the patient needs more laser treatment.
Diabetic vitrectomy
Vitrectomy is indicated in proliferative diabetic retinopathy in the following conditions:
- Non-clearing vitreous haemorrhage
- Pre-retinal (or sub-hyaloid) haemorrhage
- Tractional retinal detachment threatening, or involving, the macula
- Combined rhegmatogenous (due to a hole) or tractional (pulling action) detachment
- Progressive severe fibrovascular proliferation in spite of adequate PRP
Currently, vitrectomy for diabetic macular oedema is reserved for the few patients who have vitreous traction on the macula.
The technique is an important part of the treatment of proliferative diabetic retinopathy and leads to improvement or stabilisation of vision in 90% of patients. Vitreous and blood are cut and aspirated and membranes causing tractional detachment of the retina are removed.
The results are often poor for long-standing tractional retinal detachments of the macula. In a resource-poor environment, those with a better prognosis should be prioritised. It is worth pre-treating patients with intravitreal bevacizumab (a type of anti-VEGF) prior to vitrectomy.
A Cochrane review of six randomised controlled trials found that pre-treatment intravitreal bevacizumab resulted in shorter operations with bleeding during the operation. Post-operative reabsorption of blood was significantly shorter. Final best-corrected visual acuity was significantly better.
Treating diabetic maculopathy
Diabetic maculopathy is a major cause of vision loss amongst patients with diabetes. Treatment includes steroids, anti-vascular endothelial growth factor (anti-VEGF) and laser.
Steroid treatments
In the Diabetic Retinopathy Clinical Research Network trial, intravitreal injections of the steroid triamcinolone acetonide (IVTA), was compared with standard laser treatment. Although there were short-term improvements in visual acuity with this steroid, this improvement was not sustained. Laser was more effective and had fewer side effects than IVTA. The side effects of IVTA included cataract formation and raised intraocular pressure. Recently, the same group found that there was one exception, in pseudophakic eyes, IVTA and prompt laser seemed more effective than laser alone.
Anti-VEGF treatment
Vacular endothelial growth factor (VEGF) levels are increased in the vitreous and retina in patients with diabetic retinopathy. The increased level of VEGF stimulate the growth of new blood vessels and increase the risk of haemorrhage and further complications. Currently, there are four anti-VEGF intravitreal treatment in clinical use: pegaptanib, ranibizumab (Lucentis), bevacizumab (Avastin) and aflibercept.
Anti-VEGF treatment is currently the mainline of treatment for diabetic macular oedema with good visual outcome.
However, intravitreal anti-VEGF treatment regime is a challenging one for patients and generates a significant workload for health care providers. The financial commitments for health systems are also considerable, for example – ranibizumab injections cost around US $1,200 each and the patients may require up to eight or nine injections in the first year (a cost of around US $10,000 per patient per year). Intravitreal bevacizumab is much cheaper. In low resource settings an intravitreal bevacizumab injection can be available for as little as US $25.
In practice, laser treatment should remain the cornerstone of treating clinically significant macular oedema and the use of intravitreal injections should be tailored to the needs of individual patients.
Laser
The Early Treatment of Diabetic Retinopathy study compared macular laser with observation. There was a 50% reduction in moderate visual loss in the group that received laser (from 24% to 12%).
- Laser is not effective in clinically significant central diabetic macular oedema
- If there is no view of the fundus, laser cannot be done
- Infrequent visits are required, long lasting effect when it works
- Laser burn-creep under the fovea can also reduce vision
We must also advocate for lasers and other necessary equipment wherever there is a trained ophthalmologist.
Recommendations
- Warn all diabetes patients to come if they experience floaters or blur, as these symptoms suggest a vitreous haemorrhage
- Give pan retinal photocoagulation laser to anyone who has had vitreous haemorrhage even if there are no visible new vessels. Treat any size area of definite neovascularisation, on the disc or elsewhere. Treat any eye that has evidence of fibrosis, as this is evidence of proliferative disease
- Treat patients faster. Regression of new vessels should be seen after a week or two. If patients come from far away, consider admitting them to complete the laser before they are discharged. Attempt to complete the laser in one week, instead of several weeks. Treat the inferior retina first as new blood falls down and blocks the view inferiorly
- Make the most of each session you have. It is worth treating some patients in one session. This is particularly important if there are large neovascular formations which have an increased risk of bleeding, or if the patient is unlikely to return. Remember to avoid application of intense burns which are unnecessary to induce regression
- Repeat treatment. All neovascularisation should regress in two to four weeks. If it has not regressed, treat again. If bleeding occurs after laser, re-treat until neovascular formations have gone or maximal treatment has been given. Consider treating inside the arcades, particularly temporally.
Share this
Diabetic Eye Disease: Building Capacity To Prevent Blindness
Diabetic Eye Disease: Building Capacity To Prevent Blindness

Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free







