Setting up and Planning a Vitreo-retinal (VR) Service

Share this step
Miss Chale is a 33 year old woman who has been living with diabetes for 17 years. She lives in a rural area in Tanzania. Her diabetes is poorly controlled and she has never had an eye examination. She presented at the hospital in the city, with a history of gradual loss of vision in the left eye for 6 months. A week before she had suddenly lost all vision in the right eye.Examination showed a retinal detachment in the left eye. The macular was detached (lifted away from the layers below) and the vessels were closed. Most of the retina was covered in membranes, detached and looked very thin. Unfortunately, this eye was deemed to be beyond surgical repair. The right eye had a dense vitreous haemorrhage. A B-scan ultrasound, showed that she had a fairly localised retinal detachment and a haemorrhage.She was given an intravitreal injection of bevacizumab. 2 days later she underwent a vitrectomy in the right eye to remove the haemorrhage and given panretinal photocoagulation. Her final visual acuity was 6/18.
This case demonstrates some key points:
- Diabetic retinopathy screening needs to reach people living with diabetes over a whole region including remote areas. If Miss Chale had had access to screening and timely treatment she could have had a better outcome
- Vitreo-retinal surgery can be sight saving. Without a vitrectomy Miss Chale would be blind in both eyes.
Vitreo-retinal surgery as a sub-specialty has become a significant part of eye health systems over the last two decades, despite the high costs associated with it.
Indications for surgical management of proliferative diabetic retinopathy based on ICO guidelines (ICO, 2017)
Indications for vitrectomy
- Severe vitreous haemorrhage of 1–3 months duration or longer that does not clear spontaneously. Earlier intervention may be warranted in low- or middle-resource settings as the underlying proliferative diabetic retinopathy may have been previously untreated and highly advanced. In these settings it may be reasonable to perform vitrectomy in eyes with vitreous hemorrhage of 4 -6 weeks duration that has not cleared spontaneously
- Advanced active proliferative diabetic retinopathy that persists despite extensive pan-retinal photocoagulation (PRP). Surgery is reasonable in eyes with recurrent episodes of vitreous haemorrhage from proliferative diabetic retinopathy due to persistent vessels despite PRP or from mechanical traction on new blood vessels
- Macular detachment of recent onset. Fovea-threatening or progressive macula-involving detachments benefit from surgical management
- Combined traction-rhegmatogenous (formation of a hole or a tear) retinal detachment
- Macular oedema or epiretinal membrane involving the macula.
Surgery for proliferative diabetic retinopathy remains challenging, but improved surgical instrumentation, careful preoperative and operative planning (including preoperative injection with anti-VEGF drugs, the choice of instruments, instrument gauge and use of retinal tamponade) can provide successful surgery, often enabling meaningful visual rehabilitation even in severe cases.
To understand how this complex surgery takes place (in a case similar to Mrs Chale) watch this video on the ORBIS Cybersight website.
A vitreoretinal (VR) service should be set up in response to a demonstrable need for VR surgery and at a location where the institution has an established reputation as a referral or training centre and is providing eye care to a large number of patients. Ideally before setting up VR service there should already be an established laser treatment programme for diabetic retinopathy. Amongst the patients being treated for diabetic retinopathy will be a number who need referral for vitrectomy. There will also be other patients from the general eye clinic with retinal detachments, trauma and vitreous haemorrhages who need VR services.
Setting up a Vitreo-retinal (VR) service
VR surgery is expensive in terms of equipment, consumables and the time and cost constraints of training a VR surgeon and team away, usually away from their place of work. It is imperative that before someone embarks on training that all stakeholders are fully committed to develop this sub-speciality. This will include high ranking government and university officials who may hold the key to equipping a VR service.
Before a VR surgeon and team undergo training for VR, the institution and authority responsible for funding the institution need to commit and agree to:
- An initial investment into purchasing the expensive equipment and to procure consumables required to keep the service running
- A maintenance budget and schedule to bring in external technicians for maintenance and repair
- A budget to replace equipment that has worn out will also be required.
Essential equipment
A well established eye unit will have all the basic equipment needed to run a DR screening and treatment unit as well as an eye theatre: lasers, sterilisers, ophthalmic instruments for cataract surgery, microscopes and so on.
A VR unit requires specialist equipment:
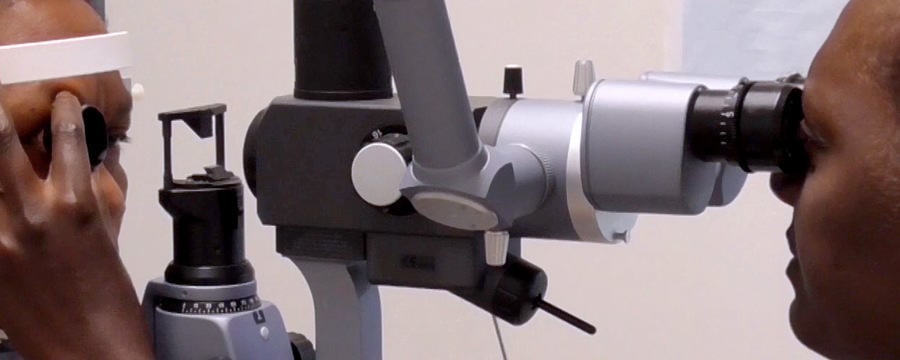
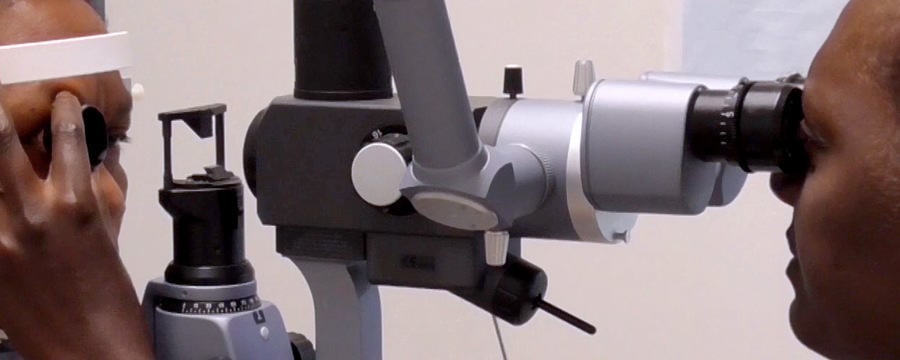
- Microscope: Needs to be capable of assistant viewing and carrying a viewing system
- Laser: There should already be a laser with an indirect ophthalmoscope for treating DR
- Vitrector: There may already be phacoemulsification equipment. When planning the purchase of phaco equipment think of the possibility of VR
- Surgical instruments for VR surgery are expensive and the team must be trained in the special care for cleaning, sterilising and protecting them
- The price of consumables is high, for example sterilisable cutters, light- pipes and other consumables which have become single use only in high resource settings.
When using the equipment it is important that an uninterrupted power supply is also available.
Vitreo-retinal fellowship training
VR surgery is a demanding surgical subspeciality, due to the delicate nature of the retina and the learning curve is steep. Candidates selected for VR fellowship training should already be skilled in all the examination techniques used to evaluate the retina. This includes slit lamp biomicroscopy and assessment with contact lenses. The surgeon also needs to be skilled in the use of the indirect ophthalmoscope and a skilled and experienced cataract surgeon. Having mastered phacoemulsification is an advantage as this teaches some of the bimanual skills that are also needed in VR surgery. While skill and experience are important, VR surgery also demands a compulsive attention to detail.
An ideal fellowship training programme:
- Is full time and hands on (not just observing), covering a wide range of clinical cases and surgical procedures
- Is structured, with a curriculum of study
- Is graded, moving from easy to complex cases. Learning how to manage complications is a critical component of fellowship training and should not be neglected
- Includes some form of assessment during the fellow ship and at the end
- Is close to home and family. This brings a number of advantages including: similar patient and pathology mix, culture, food and language and a lower cost.
The training programme can be delivered within your country or region if there is a local resident specialist providing fellowship training. If the fellow can remain in their own hospital this will have the least impact on their colleagues and the hospital’s work.
The VR team should ideally be trained to manage the VR instruments and equipment, the theatre conditions and to work alongside the VR surgeon. Where possible, it is useful for them to spend a few weeks at the fellow’s training hospital to work together.
Planning
Before a new VR unit opens, develop a strategy and plan to cope with increased theatre time and volume, ward occupation, clinic load and so on. Initially it is wise to start with the simplest cases to build the confidence of the team and the new VR surgeon or surgeons. Refer more complex cases elsewhere if possible. And plan a visit from a visiting senior VR specialist (perhaps the trainer) so that these more complex cases can be managed together. This will continue to build the experience of the local team.
What are the local challenges faced in providing vitreo-retinal surgery?
Share this
Diabetic Eye Disease: Building Capacity To Prevent Blindness
Diabetic Eye Disease: Building Capacity To Prevent Blindness

Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free







