What is a visual field?

Share this step
The visual field is the entire area (field of vision) that a person can see when both eyes are focused on a single point, straight ahead and includes what can be seen above, below, and to either side of the point the eyes are focused on. Vision is typically sharpest in the middle of the visual field. Perimetry is the examination of visual field function and is an integral part of any ophthalmic evaluation.
Visual field boundaries
The visual field (VF) is represented as a three-dimensional cone (Traquair’s island of vision). The apex corresponds to the fovea (fixation point during testing) which has the highest sensitivity to light. The base of the cone corresponds to the area of lowest sensitivity to light. The purpose of visual field testing is to define the topography of the “cone” to recognise any variation from ‘normal’.
The plotted VF (the base of the cone) extends for approximately 60° superiorally, inferiorally and nasally and 100° temporally.
 (Click to enlarge) Figure 1: Traquair’s island of vision © LSHTM CC BY-NC-SA 4.0
(Click to enlarge) Figure 1: Traquair’s island of vision © LSHTM CC BY-NC-SA 4.0
An area of visual loss within the visual field is called a scotoma. If the loss of vision is total, the scotoma is absolute; if it is partial, the scotoma is relative.
A ‘blind spot’ (labelled ‘bs’ in Figure 1) is the term used when the scotoma is absolute and is also located at the same position as the optic nerve head (approximately 15° temporal to the fovea).
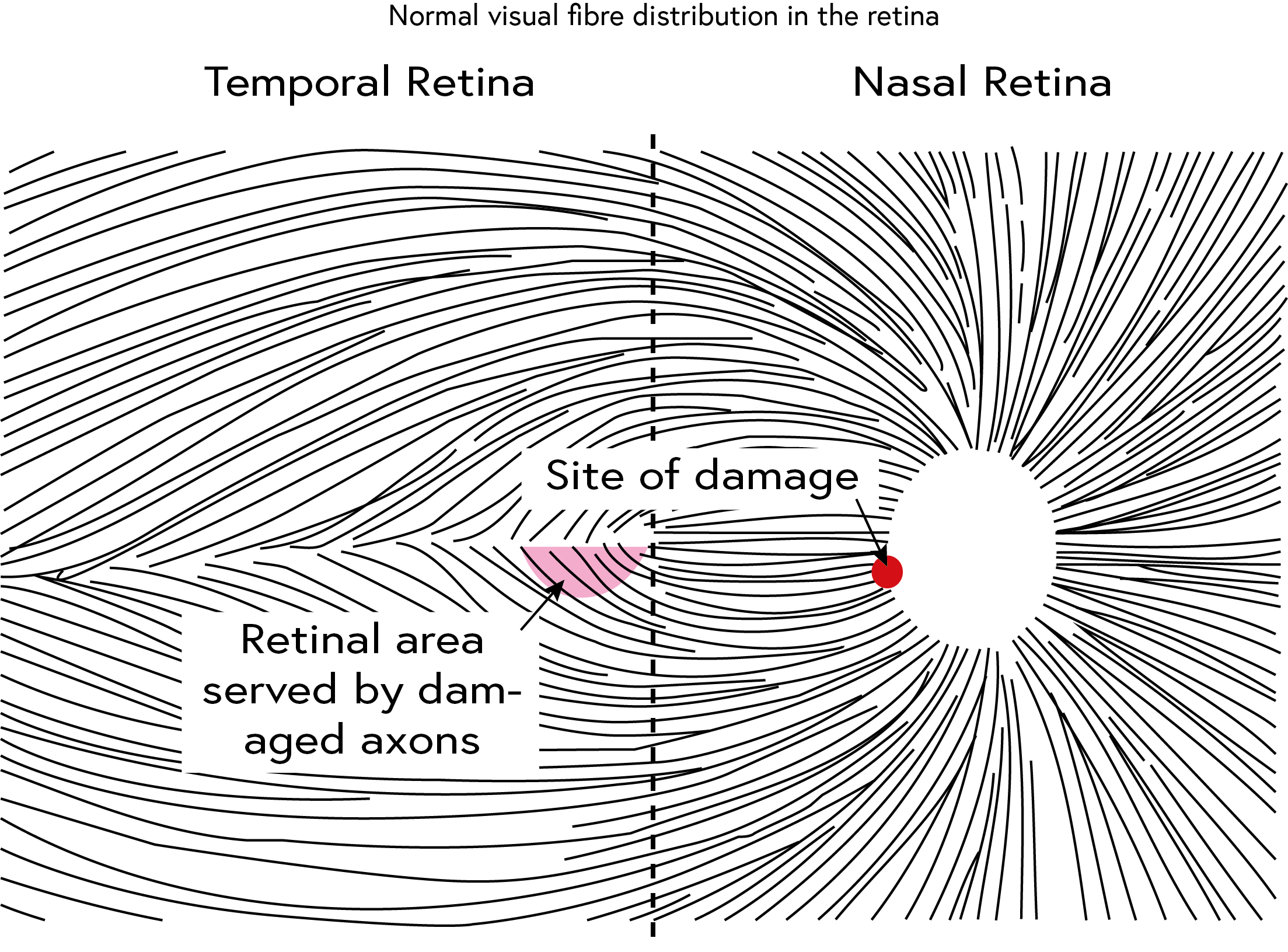
The damage that occurs due to glaucoma follows the nerve fibre arrangement in the retina (Figure 2).
 (Click to enlarge)
(Click to enlarge)
Figure 2 © LSHTM CC BY-NC-SA 4.0
Fibres that are damaged in any part of the retina (shown in pink) will have a corresponding change in the optic nerve head where all the fibres converge, this is referred to as the RNFL pattern). Glaucomatous damage typically follows the arcuate (curved) RNFL pattern. Fibres stop at the horizontal ‘raphe’ (seen as a nasal step in visual field testing).
Exploring the central visual field will reveal almost any pathology in the visual pathway, this is because the central VF (30° around the point of fixation) reflects the function of approximately 66% of the retinal ganglion cells, and its cortical representation occupies 83% of the visual cortex.
Key facts about visual field testing
- Manual and/or automated visual field testing is subjective: it is totally dependent on the cooperation and responses of the patient. Poor results that are difficult to interpret are often due to the fact that the patient either did not understand what was required or, did understand, but was unable to respond.
- Abnormalities in the visual field are a sign of damage anywhere in the visual system from the retina through to the brain’s visual cortex. Visual field defects are therefore not limited to glaucoma. A careful history and examination are essential.
 (Click to enlarge)
(Click to enlarge)
Asymmetrical visual field loss © LSHTM CC BY-NC-SA 4.0
Asymmetrical visual field loss in glaucoma can lead to late presentation as with both eyes open the patient sees no defect. Visual Field testing
- Early glaucomatous visual field defects are subtle and easily missed. Even with modern automated and sensitive visual field analysers, glaucomatous visual field loss is not evident until at least 30% of the retinal ganglion cell axons that make up the optic nerve have been lost. Progression of visual field loss in untreated glaucoma can be quite slow, and signs of deteriorating disease can therefore be missed quite easily.
- These images represent what a scene may look like to someone with different visual field defects in each eye. The left eye has inferior field loss, and the right eye has superior field loss. Because the defects do not overlap, the field defects will not be apparent when the scene is viewed with both eyes together. In primary open-angle glaucoma (POAG), the development of these defects is usually slow, and may be masked because the visual fields of both eyes overlap to produce a single binocular field.
- This means that for diagnostic purposes, it is important to test each eye separately. Non-congruous defects in each eye (e.g. a superior defect in the visual field of the right eye and an inferior defect in the left eye) could be missed when testing both eyes together as the normal areas of field in one eye overlap the defects in the other eye.
Features of glaucomatous visual field defects
Visual field loss can be diffuse (as with cataract or corneal opacification), but more commonly there are isolated defects. The visual field defects associated with glaucoma appear to be fairly non-specific, although typical loss fits with the arrangement of the retinal ganglion cell axons within the retinal nerve fibre layer of the retina.
Relatively specific glaucomatous visual field defects (see Figure 3 for examples) include:
- Nasal step defect obeying the horizontal meridian
- Temporal wedge defect
- Classic arcuate defect, which is a comma-shaped extension of the blind spot
- Paracentral defect 10–20° from the blind spot
- Arcuate defect with peripheral breakthrough
- Generalised constriction (tunnel vision)
- Temporal-sparing severe visual field loss
- Total loss of visual field.
 (Click to enlarge)
(Click to enlarge)
Examples of glaucomatous visual field defects © LSHTM CC BY-NC-SA 4.0
Examples of glaucomatous visual field defects
Types of testing:
The concept of visual field testing has been documented since the 2nd century but the technology and methods for modern perimetry was developed rapidly during the second half of the 20th Century.
Perimetry is the systematic measurement of visual field function (the total area where objects can be seen in the peripheral vision while the eye is focused on a central point).
The TWO most commonly used types of perimetry are:
1. Kinetic perimetry – this involves using test objects (fixed in size and brightness) which are moved from non-seeing to seeing parts of the visual field. The patient is required to indicate when the object becomes visible. The results are plotted on isopters, which are lines of equal differential light sensitivity.
A Goldmann visual field analyser (or perimeter) is a device that enables kinetic visual field testing and generates a permanent record of the visual field, making it a sensitive and reproducible technique, ideal for detecting change over time.
The Goldmann perimeter consists of an illuminated hemispheric bowl upon which target spots of light are shone and moved from non-seeing regions to seeing regions. During static testing, the test target can be projected at a single location and the brightness of the target object is increased until the patient responds to indicate that they have seen the target. The Goldmann device allows control of the luminance (the amount of light that is emitted from, passed through, or reflected off an object) of both the background and stimulus targets and it is important that the device is calibrated on a regular basis to ensure that individual visual field plots can be compared with others.
2. Threshold static automated perimetry – this uses test objects that vary both in size and brightness and are located in a linear sequence. The presentation of the test objects is mostly automated now and a computer algorithm controls their display e.g. a Humphreys standard automated perimetry (SAP).
Automated visual field analysers have been developed, but these are expensive and are not yet available worldwide. However, research has shown that glaucomatous visual field loss is best detected and is managed with high reliability when automated perimetry is performed. SAP machines are highly technical and require a trained person to undertake visual field testing.
You can watch this video if you wish to understand more about visual field changes in glaucoma: Visual Field changes
How to interpret visual field loss using this method is explained in the next step (Step 2.09)
As you read this article reflect on the likely functional challenges faced by patients with glaucoma when they have loss of:
a. Lower visual field
b. Extensive peripheral visual field loss
Share this
Glaucoma: A Public Health Approach to Preventing Blindness

Glaucoma: A Public Health Approach to Preventing Blindness


Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free







