Home / Healthcare & Medicine / Nutrition / Introduction to Food Science / Microbiota, diet and well-being

Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.


 Figure 1. Main Taxonomic groups of the human gut microbiota and the Domain/Kingdom Level
Figure 1. Main Taxonomic groups of the human gut microbiota and the Domain/Kingdom Level
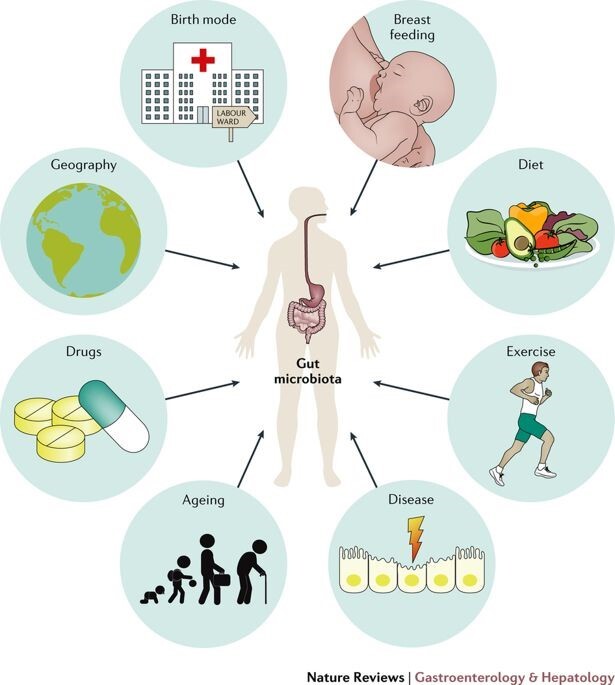 Figure 2. Major factors affecting the composition of the gut microbiome
Figure 2. Major factors affecting the composition of the gut microbiome
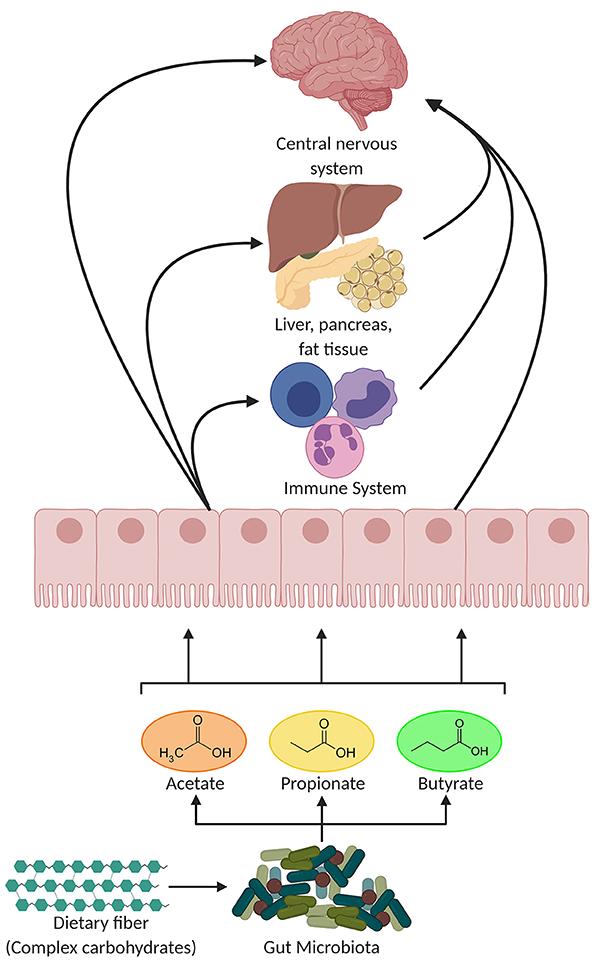 Figure 3. Main SCFAs produced by the microbiota in the large intestine through the anaerobic fermentation of indigestible polysaccharides such as dietary fiber and resistant starch. Potential pathways through which SCFAs influence gut-brain communication (Figure adapted from https://doi.org/10.3389/fendo.2020.00025)
Figure 3. Main SCFAs produced by the microbiota in the large intestine through the anaerobic fermentation of indigestible polysaccharides such as dietary fiber and resistant starch. Potential pathways through which SCFAs influence gut-brain communication (Figure adapted from https://doi.org/10.3389/fendo.2020.00025)







