The first consultation – 45 minutes
Introduction and setting expectations
- Outline the aims of the PEAK program physiotherapy consultations, which are to:
i) Educate about OA and its best-practice treatment options, so that the participant has accurate knowledge, is informed about benefits and risks of treatment and has realistic expectations;
ii) Prescribe a structured strengthening exercise program for the patient to perform at home, ideally three times/week;
iii) Prescribe a personalised weekly physical activity plan, with or without daily step goals using an activity tracker (if your patient has access to one);
iv) Equip the patient with the knowledge, skills and confidence to continue with the strength program and physical activity plan into the future after your consultations have finished, including being able to independently modify and progress the program themselves.
- Remind the patient if you have provided them with any resources (information booklets, exercise bands etc) to help them self-manage their knee OA.
- Tell them that research shows the most effective treatments for OA are self-management with exercise and physical activity, which is why the program does not involve hands-on treatments like massage.
Assessment (15 mins)
- If applicable, review the information the patient has provided in their pre-consultation questionnaire. You may wish to explore some information in further detail, or ask any additional questions not covered.
- It can be helpful to find out what the patient currently understands about OA, its prognosis and the role of physiotherapy so that you can correct any misconceptions quickly.
- Discuss with your patient their goals and expectations from treatment. Use these as motivating strategies through this and subsequent consultations. You may need to help your patient refine their goals to ensure that the goals are relevant to the knee problem and amenable to physiotherapy care.
- Choose some questions from your subjective assessment (or the pre-consultation questionnaire) that may be suitable for re-assessment in future consults.
- Objective assessment should focus on tests and tasks that will help you determine the most appropriate strengthening exercise program, and to tailor a physical activity plan for the patient. Observation of functional tasks such as walking, stair climbing, squatting, sit-to-stand etc. are helpful and can also be done readily via video consultations. Simple balance tests can be helpful also- consider patient safety especially during video consultations and ensure the patient has a stable chair or bench for support if required.
- Consider choosing a functional task or two that may be useful for future re-assessment (we often re-assess sit to stand in our research studies).
Education (10 mins)
It is important that your patient has accurate knowledge about OA and its prognosis, including the beneficial role of exercise and physical activity, before embarking on an exercise program. It is also important that the patient understands that exercise and physical activity are recommended by experts, based on research evidence, as a core and fundamental component of high-quality OA care. You may like to begin by inviting the patient to “Tell me what you know about osteoarthritis” as a way of initiating discussions. The “Osteoarthritis Information” booklet (available in the Resources section for learners who choose the course upgrade option) contains a variety of useful information about OA and its treatment options, presented as a high-quality booklet in user-friendly language. You may wish to provide this to your patient, and/or focus your discussions around the content within the booklet. Whilst discussing OA, its prognosis, and the benefits of exercise (particularly relevant to other treatments), you may also need to correct any inaccurate knowledge or misconceptions that the patient may have.
Strengthening exercise program (15 mins)
Based on the information gained from your assessment, and in discussion with the patient about which exercises they feel they can manage, you should aim to provide a strengthening exercise program (we suggest three exercises initially) from the exercises in the “Exercise Booklet”. Ask the patient to refer to their copy of the booklet (if you have provided them with one), so they can help make the decision about which exercises they feel they will be able to manage and adhere to. In this first consultation, you should aim for a program comprising-
- One quadriceps exercise
- One hip abduction exercise
- One hamstring exercise
Teach your patient how to perform each exercise. You should aim to:
- Watch the patient perform each exercise themselves and correct their technique if necessary. Ideally, you should watch the patient complete one set of each exercise .
- Prescribe a dosage for each exercise. The strengthening exercise program should, ideally, be performed three times each week by the patient. However, the number of sets and repetitions to be performed is at your discretion, and this may differ for each exercise prescribed. The exercises, and the level of intensity should be chosen on the basis of the assessment, and what you observe as the patient performs a set of the exercises during the consultation.
- Tell the patient how many reps and sets of each exercise they should perform.
- The patient may wish to use the “Knee Plan and Log Book” (available in the Resources section for learners who choose the course upgrade option) to record for themselves what you have advised them to do.
- Patients may also monitor and record their exercise performance in the log book section of the “Knee Plan and Log Book” until the next consultation so you can review their progress.
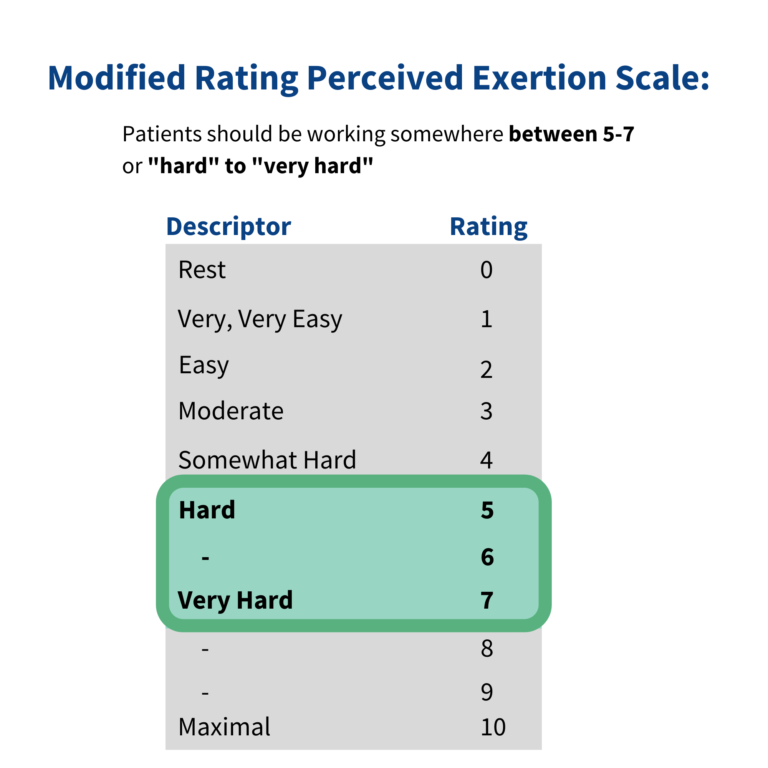
To assist you in choosing which level of exercise may be most appropriate, and in setting the appropriate exercise dosage, you should watch the patient perform a full set of reps of each exercise to determine how hard it is for them to perform the exercise. Ideally, each exercise should feel “hard” to “very hard” to perform. If the patient reports the exercise was “easy”, “moderate” or “somewhat hard”, the exercise and or dosage may not be challenging enough and modification may be required.
It is important the patient understands that it can be normal to experience some knee pain while performing the strengthening exercises. The patient also needs to know how to identify a pain flare-up and how to manage it.
Exercising with knee pain
- It is normal to experience some pain/discomfort during the exercises. In fact, FEELING SOME PAIN DURING EXERCISE MAY HELP reduce knee pain in the long-term
- Your knee is painful because it has become deconditioned and is not used to movement. Pain is NOT a sign that the exercises are causing tissue damage. You need to exercise your knee, so it will become strong and enable you to do what you need/want to do.
- Remember that it is normal to feel some soreness in the muscles for a few days when you start exercising or when you increase the intensity. This is actually a good sign as it means you have been working the muscles.
Doing painful exercises may change the way your brain processes pain and the way you think about pain, helping you to re-start movements that were previously fearful of.Exercise triggers the brain to release chemicals (endorphins) that have an analgesic (pain-relieving) effect- exercising at an intensity that causes some pain may release more endorphins than pain-free exercise.
Managing a flare-up of knee pain
- If the pain during the exercises is more than you find acceptable, or flares up for longer than 24 hours after the exercises (or causes increased knee swelling), then decrease the amount of exercise until you’re coping with it again. You can do this by: i) Reducing the dosage (by decreasing the number of sets and/or repetitions) until the flare-up has settled, and then gradually increase dosage again ii) Changing the colour of the elastic band to provide LESS resistance iii) Trying any of the easier variations described underneath the exercise iv) Stopping the exercise that caused you pain, and replacing it with a different exercise from the booklet once the flare-up has settled
- Talk to your physiotherapist during your next consultation so that the exercises can be reviewed and modified if necessary.
- Don’t stop all the exercises completely as complete rest is unlikely to solve the problem.
Physical activity (5 mins)
In preparation for setting a personal physical activity plan in the next session, it is important to obtain a baseline indicator of your patient’s weekly physical activity. If your patient has an activity tracker (e.g. Fitbit, pedometer, Garmin etc), ask your patient to record their daily step count over the next week. This way, you can set a realistic and achievable step goal as part of the physical activity plan at the next session. They can record their step count each day in their Knee Plan & Log Book (available in the Resources section for learners who choose the course upgrade option). If they don’t have an activity tracker, you can ask them to take note of any physical activity they undertake over the next week, including the amount/duration (e.g. how many times they went for walk, how long far or how far).
Concluding the first consultation:
To get the most out of educational discussions, it is helpful if the patient can do some pre-reading. That way they can consider any questions they may have, and can be proactive about discussing with you any information that they didn’t understand. In the next consultation, education will focus on physical activity, so you might like to encourage the patient to read the relevant sections of the “Osteoarthritis Information” booklet (available in the Resources section for learners who choose the course upgrade option).
Do you like to regularly provide educational information to patients that they can read between sessions? What do you think are some of the pros and cons of this approach? Comment below to join the discussion.
Share this
Physiotherapy Exercise and Physical Activity for Knee Osteoarthritis (PEAK)

Physiotherapy Exercise and Physical Activity for Knee Osteoarthritis (PEAK)


Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free







