Follow-up consultations – physical activity
Physical activity program
In consultation 2, aim to discuss and agree on a personal physical activity plan for your patient. This involves the following key aspects:
- Review the patient’s baseline physical activity (which you asked them to monitor over the previous week)- this may include a daily step count based on an activity tracker (if they own one) and/or a discussion of the types/amounts of physical activity the patient has engaged in over the prior week.
- If appropriate, set a daily step goal on the basis of this information and discussion with the patient, ensuring it is realistic and achievable. It is OK if the goal is to MAINTAIN daily steps (eg in the case of someone already taking >10,000 steps/day). For many patients, however, you will want to aim to increase the daily step count. Note that a threshold of 6,000 steps/day seems to best discriminate between people with knee OA who do and do not develop functional limitations two years later, so this could be a useful goal for some patients.
- For all patients, agree on a personal (daily or weekly) physical activity plan, that will help them achieve the step goal and/or help them to increase the amount/intensity of physical activity they regularly undertake. Again, it is OK to set a plan that MAINTAINS physical activity levels if the patient is already sufficiently physically active.
Ensure you discuss and agree upon a physical activity plan with your patient that suits their individual needs and goals.
- Encourage the patient to complete the physical activity plan template in the “Knee Plan and Log Book” (available in the Resources section for learners who choose the course upgrade option) – so they know exactly WHAT they should do, WHEN and for HOW long.
- Encourage patients with a step goal to record their progress in the “Knee Plan and Log Book” each week, until the next consultation.
- Ask your patient to think about potential barriers to their physical activity plan and think of potential strategies for overcoming barriers (discuss some ideas contained in the “OA Information” booklet available in the Resources section for learners who choose the course upgrade option). People are much better at dealing with set-backs if they plan ahead and have some clear strategies to help overcome them in the first place!
Recommendations for good health:
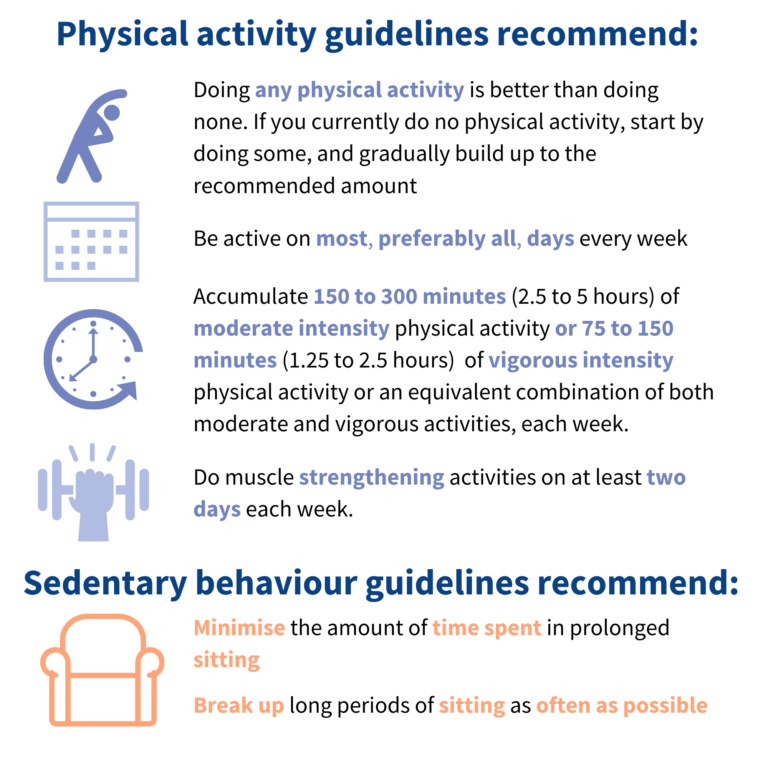
Australia’s Physical Activity & Sedentary Behaviour Guidelines for adults aged 18-64 advise that being physically active and limiting your sedentary behaviour every day is essential for health and wellbeing. The guidelines are for all adults aged 18 – 64 years, irrespective of cultural background, gender or ability.
Australia’s Physical Activity & Sedentary Behaviour Guidelines for Older Australians (65 years and older) advise that being physically active and staying fit and healthy will help you to get the most out of life, whatever your age. These recommendations are designed to help older Australians achieve sufficient physical activity for good health as they age. They are mainly for people who are not currently building 30 minutes of physical activity into their daily lives and are looking for ways to do so. Being physically active for 30 mins every day is achievable and even a slight increase in activity can make a difference to health and well-being.
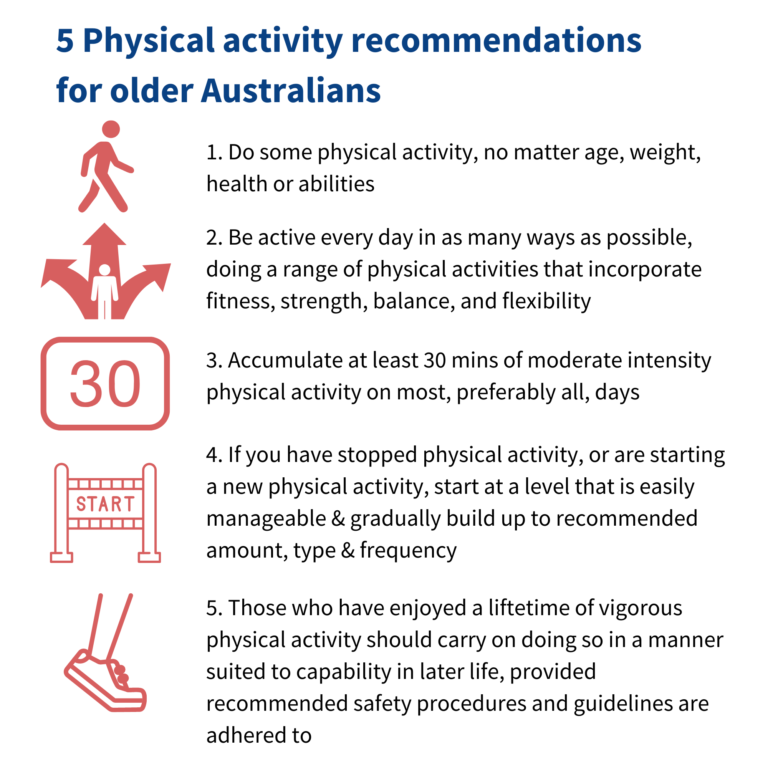
How intense does the activity need to be? For good health, people should spend some time on most days being physically active at moderate intensity. However, if this is too difficult for your patient at first, health benefits can still be gained by doing more light physical activity and less sedentary activity. Therefore, the focus should be on increasing the amount of general physical activity you do, regardless of the intensity.
One way to gauge the intensity of physical activity is to get the patient to think about how hard they are breathing. If they are breathing harder than normal but still able to speak in sentences, then they are working at a moderate intensity. If they are out of breath and can speak only one word at a time, then their intensity is probably vigorous! If they don’t even have to breathe deeper or faster, then they are probably working at a light level.
Benefits of a regular and ongoing physical activity plan
Will help patients manage their knee OA symptoms, lose weight (if required), feel better and, of course, has all the other added general health, well-being and disease prevention benefits. Physical activity plans will be highly varied and individualised in terms of content, frequency, timing and intensity. Below are some general principles with which to guide your conversations about physical activity plans:
- Anything is better than nothing. Everyone can benefit from doing more physical activity (apart from some extremes). However, people who go from doing nothing to a little bit of activity gain more benefit than people who go from doing a lot of physical activity to doing a little bit more. That means any small increase is worth it, particularly if they are already doing very little.
- Don’t set someone up to fail. Remember not to impose your own agenda onto the patient. Also make sure the patient is not being overly ambitious about what they can achieve. Start with easy goals so patients achieve success and then BUILD HABITS as well as skills in planning and problem-solving.
- Create positive expectations about physical activity. Your compassion and empathy, as well as your optimism for success, will increase likelihood of achieving success and positive outcomes. Reinforce that no harm is being done to painful joint(s) even if some pain is felt, and that joints will do better in the long term when used and loaded. Consider using stories of other people’s successes.
- Variety is the spice of life. People can do several different types of activity during any week, mix it up and change over time. Discuss a range of options to consider now or in the future. Explain that all different types of activities can provide benefits (e.g. housework, playing with children, walking to shops).
What types of general physical activity may be suitable?
Here are some ideas you could consider discussing with your patient:

Tips for helping your patient increase general physical activity levels
- Small changes to your daily routine can have a positive effect on your overall health as well as your knee osteoarthritis.
- Avoid long periods of inactivity in your day.
- More frequent short bouts of activity work best for people with knee osteoarthritis.
- Perform physical activities over realistic timeframes.
- Gradually increase your physical activity and/or make it harder.
- Vary your activity by changing the environment (eg walking in water or at the local park instead of around the block).
- Pace your activities- even on bad days.
- Time yourself to help you pace your activity and make sure you don’t over- or under-do it.
- Use the activity tracker provided by the study to record how many steps per day you take.
- Perform moderate intensity activity in bouts of at least 10 minutes. That means you are puffing for 10 minutes continuously.
- If appropriate, encourage your patient to access local exercise facilities in their community e.g. the gym, local walking group, local pool. Help them locate the services and facilities they require by searching the Web for facilities/services in their area.
Evaluating progress over subsequent consultations
From consultation 3, you should review progress on the personal physical activity plan you agreed on at the prior session and modify it/progress it as appropriate. This involves the following key aspects:
- If physical activity goals were achieved- congratulate the patient and identify strategies that helped them be successful.
- If physical activity goals were not achieved, discuss reasons why, reconsidering if the goals were too ambitious or if unanticipated barriers got in the way that the patient did not know how to deal with.
Some prompts that may be useful in reviewing and progressing the physical activity plan:
How did you go trying to increase your overall daily physical activity levels?
Did you meet the goals we discussed last time?
What strategies did you try in order to increase your daily steps?
What worked for you? What didn’t’ work?
Are there any aspects of the physical activity plan you want to change for the upcoming few weeks that will make it easier for you to meet your physical activity goals?
Do you feel ready to progress your goals, or do we need to set more realistic goals for the next few weeks?
Share this
Physiotherapy Exercise and Physical Activity for Knee Osteoarthritis (PEAK)

Physiotherapy Exercise and Physical Activity for Knee Osteoarthritis (PEAK)


Reach your personal and professional goals
Unlock access to hundreds of expert online courses and degrees from top universities and educators to gain accredited qualifications and professional CV-building certificates.
Join over 18 million learners to launch, switch or build upon your career, all at your own pace, across a wide range of topic areas.
Register to receive updates
-
Create an account to receive our newsletter, course recommendations and promotions.
Register for free







